Critical Incident Analysis in Patients with Mental Health Issues
Introduction
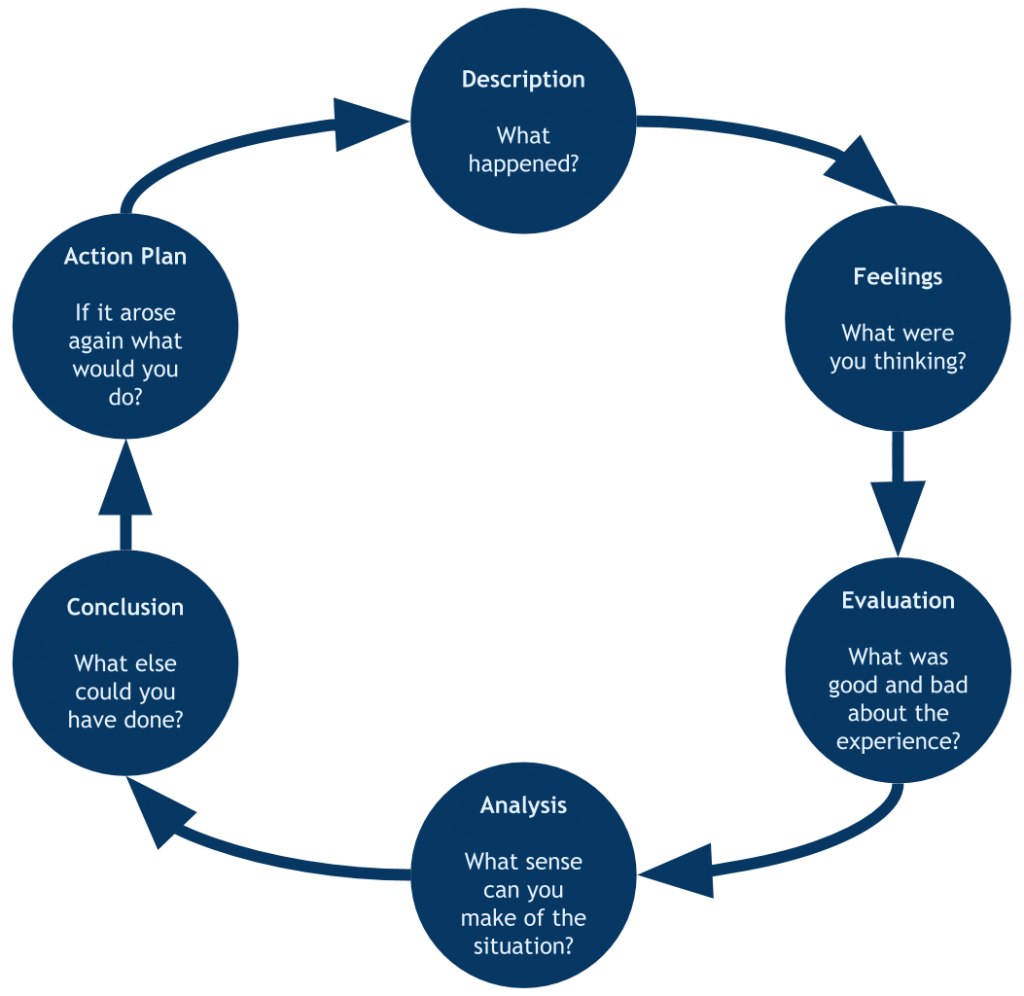
The ongoing pandemic is associated with an increase in mental health problems, especially among people who live alone. This is especially the case for older people who are more likely to experience social loneliness during the pandemic. Public health strategies to address the mental health needs associated with these problems are therefore needed. While in most cases, family members take the responsibility of caring for individuals with mental health issues; individuals who live alone within the community are exposed to adverse health outcomes since they lack appropriate care. The lack of social support, especially for older people, is associated with poor health outcomes. In such cases, safeguarding policy applies, where healthcare providers are required to prevent the neglect or abuse of vulnerable adults. This paper incorporates a critical incident analysis of the actions taken to address the needs of an old and frail man, whose quality of life has been deteriorating due to the lack of appropriate care. The Johns model for structured reflection is used to guide the critical analysis, which is based on five cue questions which will help in breaking down the experience and reflecting on the process and the outcomes.
Context of your practice experience
Healthcare providers are in a unique position to identify individuals who need safeguarding. Critical incidents in healthcare are common; they are either negative or positive. In this paper, the critical incident being analysed was positive, whereby the patient benefited from the resulting actions. The practice experience to be included in this paper incorporates aspects of mental health nursing. While any adult is at risk of becoming vulnerable due to various reasons, including illnesses and ageing, some individuals are often in particular risks due to their social circumstances. This means that a nurse ought to be able to identify the factors that contribute to an individual’s vulnerability (Straughair, 2011). According to the Nursing and Midwifery Council (NMC) (2018), safeguarding involves protection of individuals from harm, including physical, emotion, sexual, or financial harms and neglect. Safeguarding vulnerable adults is a crucial part of nursing practice. There are instances when nurses are unsure of their roles in safeguarding vulnerable adults, especially within the community (Fanneran, Kingston and Bradley, 2013).
The first phase of Johns model of reflection involves describing the incident, establishing what contributed to the problem, and background of the experience. Therefore, the critical incident that I experienced involved Mr Walsh, a 65-year-old divorced man who lived alone in the community. The patient was frail, which could be associated with self-care deficits. He had a prescription of antidepressants, which he had stopped taking due to the fear of intentional overdosing. The patient made constant threats of taking his life. This incident is vital in nursing practice because according to the NMC Code, nurses have a responsibility to implement interventions to support individuals who have signs of self-harm and suicide ideation. These problems can be attributed to the fact that Mr. Walsh has recently divorced his wife. Divorce is associated with an increased risk for depression as well as suicide thoughts (Stack and Scourfield, 2013). The fact that the patient is taking antidepressants means that he has depression; another reason why he needed to be admitted. Patients with depression often have suicidal thoughts and self-harm behaviours (Munro and Milne, 2020). Signs of self-neglect were also visible, with the patient showing lack of medication adherence which was worsening Mr. Walsh’s condition.
Overview of your critical incident
On vising Mr. Walsh together with a social worker, we established that it was in his best interest to admit him since his frail condition and the fact that he lived alone meant that he needed to receive medical services promptly. The local authority in the patient’s community explained that Mr. Walsh has been living alone for several months, and has completely neglected himself. During the pandemic period, he left his door unlocked for visitors. A trigger for action was raised when some come community members expressed their concerns over his overall quality of life. On notifying the social work office, the social worker visited the patient and established his need for further care. I visited the patient together with the social worker. A risk assessment was performed, and together with the multidisciplinary psychiatric team (MDT), it was identified that Mr. Walsh was at risk of endangering himself. His depression seemed to be worsening, which can be attributed to suicidal ideations. The patient was, however, in a position to make decisions regarding his welfare; hence he consented to the decision to admit him. It is the responsibility of individuals dealing with such a patient to respect the patient’s right to make his own decisions regarding his care. A discussion was, therefore held with the patient where he was informed that his health was at risk. The patient was provided with information about the options available for his protection and how to minimise harm. He then consented to the admission though informally.
Critical analysis of the safeguarding decision, related to key literature and evidence
In the second phase of John’s model of reflection, is about reflection. In Mr. Walsh’s case, the decision to admit him was made in an attempt to protect him from harming himself. Once it was identified that the patient was at risk due to health and social care deficits, a decision to safeguard him was made. The approach was based on the safeguarding policy and the Mental Health Act (MCA) of 2005 which focus on empowering and protecting people who have limited capacity to make decisions for themselves or have an increased risk for self-harm (Social Care Institute for Excellence [SCIE), 2009). This action benefited the patient as it led to better health outcomes. On a personal perspective, the actions taken during the experience were fulfilling, as I had acted according to the principles of the nursing profession. The action involved a team of individuals from the community, and while I cannot explain their feelings concerning the experience, the outcomes highly likely led to positive feelings among other members of the MDT.
Various factors (internal and external) influenced the decision that was made to admit the patient. Given the patient’s home environment and health, it was established that the patient had minimal ability to care for himself, hence needed social and healthcare support. The decision was also influenced by the safeguarding policy. When making this decision, various sources were consulted, including the safeguarding policy, the MCA, mental health act and the local safeguarding authorities. The local safeguarding authorities participated in the risk assessment process while the other three sources provided information relevant to the care of patients such as Mr. Walsh. Consulting these sources impacted the decision to admit the patient, as they all supported the notion that he needed support care services.
The six principles of safeguarding, including empowerment, protection, prevention, proportionality, partnerships, and accountability, were considered during the critical incident. Even though it was evident that the patient had limited capacity to make own decisions, according to the MCA of 2005, it was our responsibility as healthcare professionals to ensure that the patient was empowered to make his own informed decisions. The Act also asserts the need to make a decision for a person who lacks full capacity in their best interest. In this, the decision to admit the patient was made based on the fact that his health was at risk, and he was vulnerable. Additionally, the patient was encouraged to participate in the decision-making process, since the Act requires those making decisions on behalf of others to encourage the individual to participate in any act or decision affecting them. The MCA asserts that it is wrong to assume that an individual cannot make a decision because of certain health conditions. Involving a patient in the decision-making process is paramount. Patients are experts in their values and beliefs, while healthcare professionals are experts in health-related concepts. This, therefore, emphasises the importance of collaboration with the patient during the decision-making process. It is, however, critical to ensure that the patient has decisional as well as executive capacity, as this guarantees the ability to participate in the decision-making process (Braye, Orr and Preston‐Shoot, 2011).
The purpose of admitting the patient to the psychiatry ward was to ensure that he was protected from harming himself. This action prevented harm, and it was proportional to the risk identified. By working with the social worker and community members, partnerships in care provision were established, and these promoted positive results. Ensuring the safety of a patient cannot be managed in isolation, hence partnering with the patient, and partner agencies is vital in improving the outcomes of the safeguarding activity (Braye, Orr and Preston‐Shoot, 2011). When a patient who needs safeguarding has been identified, it is vital to concentrate on improving life for the person concerned. Additionally, raising the awareness of communities to work alongside professionals is vital, especially if one is dealing with a patient within the community. For Mr. Walsh, his problem is self-neglect, which can be attributed to his social life. Considering human rights, safeguarding patients who present with self-neglect can be difficult. However, evidence of self-neglect can prompt a safeguarding inquiry, leading to other forms of social care intervention (Braye, Orr and Preston‐Shoot, 2011). Considering these concepts, therefore, the decision to safeguard Mr. Walsh through admission to the psychiatric ward was based on his inability to care for himself, evidence of medication nonadherence, and suicidal thoughts. Throughout the process, the patient’s confidentiality was maintained, as his information was only visible to the authorised individuals, including the local social work offices and the healthcare professionals responsible for his care.
As healthcare providers, it was our duty to conduct a safeguarding inquiry. When making the decision to admit him various factors were considered, including his needs for care and support, his risk for self-neglect, the impact of this decision on his wishes, and the potential for increased risks. Although the decision to admit the patient was in his best interest and resulted in positive health outcomes, there are various areas that could have been improved. For instance, an effort was not made to identify whether there the patient has any relatives within the community who could participate in his care process. Involving family members in the care process would have made the care process easier. Having left out this part of care, I feel that all options were not considered. However, the option selected was beneficial for the patient, and it was in his best interest.
The identified areas of improvement provide a learning opportunity, especially in safeguarding patients who are vulnerable within the community. This experience changed my perspectives regarding MDT and collaboration between care team members. Grim (2019) asserts the importance of shared decision making (SDM), especially in mental healthcare. I now value working together with individuals from different professionals, as this is associated with better patient outcomes. I feel that this experience was a learning opportunity, and presented with the same situation again, I would handle it better by ensuring that adequate inquiry on the patient’s relatives is conducted. This will ensure that a partnership between the patient’s family and the interprofessional team yields a positive patient care experience. This experience changed my aesthetic knowledge, and now I view my role as a mental health nurse as not only being confined within healthcare facilities but also being responsible for ensuring the safety of vulnerable individuals within the community.
Voice of the adult/child/relative and their experiences
Service users should be viewed as carriers of knowledge and equal collaborators (Grim, 2019). Involvement of service users in the decision-making process is vital in health and social care policy (Wallcraft, 2012). The patient provided informed consent for admission, and since he was living alone, he cited that he had lost all hope; hence he did not value the importance of caring for himself or adhering to medication. Mr. Walsh believed that he did not deserve being alive, another indication that the patient had an increased risk of harming himself. His assertions provided further evidence to support his admission. He explained that his previous experiences with the healthcare system were negative, since any time he reached out for help, he was dismissed. His concerns in this particular incident were having us as his healthcare team believe him because this would be a form of motivation for him to keep living, listening to his complaints revealed to us that the patient was suffering from a form of depression that required urgent psychiatric care. When delivering patient care, listening to the patient reveals critical information that can direct the care approach to be taken.
Impact of the incident on your practice
Though the analysis of this critical incident, I have learned the importance of safeguarding vulnerable individuals and the role that nurses play in this process. Moving forward, I will focus on enhancing my inquiry skills, as these are important in nursing practice. Inquiry helps a nurse to uncover information about a patient, which can be beneficial in the care process. The experience also improved my ability to collaborate with professional team members for the benefit of the patient. Additionally, including patients in decisions affecting their life is vital in demonstrating respect for patients’ dignity and autonomy. Curiosity is a vital concept in nursing practice that moving forward I plan to develop. In future, I will focus more on understanding patients from their own perspectives of the world, while delivering care according to the principles of nursing practice.
Reflection and recommendations for future development
The reflection has revealed various aspects of care that are vital in nursing practice, and I will ensure that I consider these aspects in my future practice. As a nurse, I have the responsibility to recognise patients’ vulnerability and to ensure the protection of vulnerable adults. The analysis shows that the experience was vital for my development as a nurse. Given the importance of in safeguarding patients and the role of nurses in this process, I plan to enhance my safeguarding skills by enrolling for adult safeguarding training. This will improve my skills in adult protections, and consequently, I will be able to provide efficient care to vulnerable patients within the community.
Conclusion
Protecting vulnerable individuals is an essential part of nursing practice. Critical incidents in healthcare are common, and reflection of critical incidents is viewed as an important learning tool in nursing. The practice helps in bridging gaps I theory and practice, by allowing a nurse to explore actions and feelings while examining literature. Nurses play a significant role in the protection of vulnerable adults, and through the analysis of a critical incidence involving safeguarding a vulnerable adult, I learnt the importance of a multidisciplinary approach when dealing with patients. Additionally, involving a service user in the decision-making process is vital as is demonstrates the respect for an individual’s autonomy. Safeguarding a vulnerable adult requires that a nurse understand the factors associated with the individual’s vulnerability and how these factors affect the overall quality of life of the patient. A reflective critical analysis is important in helping nursing professionals improve their practice.