Chronic kidney disease
CKD is also known as chronic kidney failure. The kidneys gradually lose their function in CKD. Kidneys normally filter waste and excess fluids from a person’s blood. The waste and the excess fluid are then excreted in the urine. An individual’s body may accumulate electrolytes, harmful amounts of wastes, and excess fluid as CKD progresses. There are five stages of CKD. Stage 1: kidney damage occurs with or without an increase in GFR. Stage 2: there is a slight decrease in GFR 60-89 (UCLA Health, p. 1). Stage 3: GFR ranges from 30 to 59. Stage 4: severe reduction of GFR 15 to 29. Lastly, stage 5: GFR less than 15 with kidney failure.
Etiology
High blood pressure and diabetes are the most common causes of CKD (Cleveland Clinic, p.1). High blood pressure can harm the blood vessels in the kidneys, making them lose their normal function. When the kidneys’ blood vessels are damaged, they may not function adequately, or they may not eliminate waste and excess fluid from the body. This can lead to a more rise in blood pressure resulting in a dangerous cycle. DM is characterized by high amounts of glucose in a person’s blood, which can cause damage to kidney filters. As time goes by, kidneys become so weak that they cannot absorb excess fluids and waste from the blood.
CKD can also be caused by; malformations that occur while a baby is still in the womb. Urine outflow may be prevented due to narrowing making urine have a backflow to the kidneys. Polycystic kidney disease is an inherited condition that causes large cysts in the surrounding tissues and the kidneys. Glomerulonephritis causes damage to the kidneys filtering units (Cleveland Clinic, p.1). Lupus and recurrent UTIs may also cause CKD. In addition, CKD can be caused by obstructions like an enlarged prostate or renal calculi.
Clinical signs and symptoms
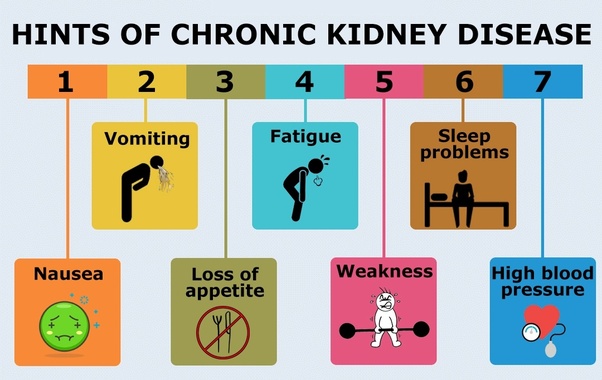
Some individuals may not show the signs of CKD; however, they may appear gradually. Patients may complain of sleeping difficulties, loss of appetite, headache, general body weakness, muscle pains, and fatigue (CDC, p.1). Other symptoms may also include nausea and chest pains due to fluid build-up around the heart.
CKD signs may include swelling of the ankles and legs. On examination, there would be a decreased pulse rate, tachycardia, and high blood pressure. The veins in the neck may also be distended (CDC, p.1). Crackles may be heard on auscultation as a result of pulmonary edema. Besides, bruises, poor skin turgor, linseys nails, and excess itching may also be seen in a CKD patient.
Lab findings
Urinalysis is one of the lab tests done in CKD. Findings may show the presence of protein and blood in the urine. Albumin may also be present in CKD patients. Urine albumin-to-creatinine Ratio greater than 30mg/g indicates CKD. GFR tests can also be done, and a GFR of less than 60 indicates CKD (UCLA Health, p.1). The HB level in a full hemogram may be low due to anemia. Serum creatine levels and blood urea nitrogen may also be elevated in CKD.
Imaging studies
In CKD, different imaging studies can be performed. These include; a kidney CT scan; it can define masses or cysts that may be detected in a normal ultrasound. Renal calculi causing CKD may also be seen in a kidney CT scan (Cleveland Clinic, p.1). Renal ultrasound; some of the positive findings may include; fluid collection, infection, tumors, abscesses, or cysts. X-ray of the kidney can also be done, which may show kidney enlargement due to fluid retention.
Differential diagnosis
Some conditions may present in a similar way to CKD; therefore, it is important to rule them out to avoid missing out on CKD diagnosis. These include; acute kidney disease; it may present in a similar way to CKD, but it’s of sudden onset (UCLA Health, p.1). Unlike in CKD, the kidneys in AKI may stop carrying out their normal functions suddenly. Nephrolithiasis: hard deposits in the kidneys cause obstruction in nephrolithiasis. Signs and symptoms may be similar to CKD, such as nausea, loss of appetite, and vomiting. The difference is that there is no loss of function in nephrolithiasis.
Treatment
Since chronic kidney disease has no specific cure, the primary goal of treatment is to prevent disease progression, alleviate signs and symptoms and control any underlying conditions that may worsen the condition. If a patient has high blood pressure, Bp medication can be administered. This may include an ACE or angiotensin II receptor blocker, which will help regulate the blood pressure to avoid the disease’s worsening (Cleveland Clinic, p.1). Medication to lower cholesterol levels such as statins. This may be prescribed because patients with CKD may have elevated cholesterol levels which may cause other complications like heart failure. Drugs to control anemia; may include erythropoietin supplements which help in alleviating anemia symptoms in CKD.
Drugs to minimize swelling/edema; edema in CKD may occur due to fluid retention. Diuretics can be prescribed in CKD to minimize edema and maintain fluid balance in a patient’s body. Supplements such as calcium and vitamin D can also be given. These drugs aid in the prevention of bone weakness and the reduction of the risk of fractures. At the end stage of CKD, dialysis can be recommended. Dialysis aids in the removal of excess fluid and waste when a patient gets kidney failure (National Kidney Foundation, p.1). In severe cases of CKD, a kidney transplant may also be recommended. CKD can also be managed non-pharmacologically by advising patients to limit their protein intake.
Prognosis
The severity of CKD may vary. CKD may worsen over time, but treatment has been shown to minimize the disease progression and prevent further complications. If left untreated, CKD may cause other complications like kidney failure or cardiovascular diseases (National Kidney Foundation, p.1). The majority of CKD patients die when they reach end-stage renal disease. A patient may also get conditions like anemia which may worsen CKD. The risk of mortality may go high if a patient gets complications like cardiovascular issues or other complications associated with CKD.
Conclusion
CKD is a condition where kidneys gradually lose their function. It is also known as chronic kidney failure. There are five stages of CKD, and the GFR varies in each stage. CKD can be caused by high bp, diabetes, recurrent UTI, polycystic kidney disease, and malformations that happen while the baby is still in the womb. Signs and symptoms may include; fatigue, nausea, body weakness, edema, and headache. Various conditions may present in a similar way to CKD; therefore, physicians must take a detailed history and carry out the appropriate tests to avoid missing out on CKD diagnosis, which may cause complications if not properly managed. If CKD patients are properly managed, complications may reduce, and the risk f mortality may also reduce.