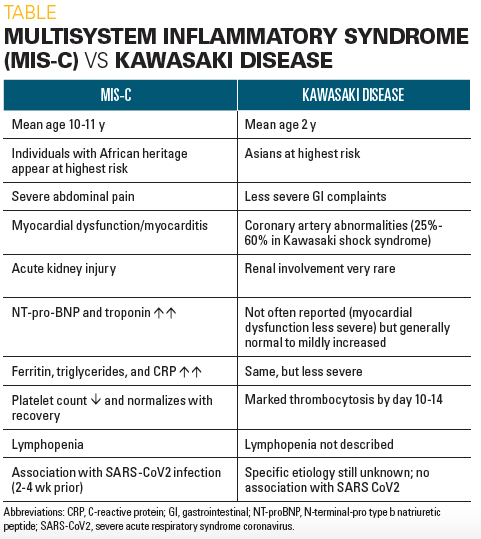
Multisystem inflammatory syndrome represents a condition that shares a description much like that of Kawasaki disease. Kawasaki disease is a large and medium-sized vasculitis affecting infants and children usually younger than four years old and characterized essentially by coronary artery involvement and mucocutaneous manifestations (Burns and Glodé, 2004). As a new entity, the multisystem inflammatory syndrome was previously described as “Kawasaki-like” (Esteve-Sole et al., 2021). It is a manifestation of SARS-COV-2 infection in children which before then was thought not to affect children. Multisystem inflammatory syndrome in children (MIS-C) can be described as a Kawasaki like syndrome seen about 4 weeks after the peak of SARS-COV-2 infection and presenting with higher incidences of gastrointestinal and neurological manifestations, myocarditis, and cardiac involvement (Godfred-Cato et al., 2020) Generally, MIS-C appears to have a greater prevalence and affects mostly older children.
Further description of MIS-C defines 3 classes; class 1 or true MIS-C with more severe neurological and gastrointestinal manifestations; class 2 which is associated with acute SARS-COV-2 infection; and class 3 which is phenotypically similar to Kawasaki disease (Godfred-Cato et al., 2020). It is notable that because of the novel nature of the disease a likely diagnostic criterion has only just been described based on earlier cases of the syndrome but there is still a lack of specific biomarkers. Lymphopenia, leukopenia, thrombocytopenia, and increased ferritin are among the notable lab features that have been determined (Morris et al., 2021). Unlike Kawasaki disease whose pathogenesis and underlying mechanisms are fairly
known, MIS-C has only been hypothesized to involve cytokine action at a grand scale. Tied to an also seemingly novel disease entity that is SARS-COV-2 infection, causing Covid 19, there is far more still to be understood about the mechanisms leading to this disease that is considered to be somewhat uniquely different to the Kawasaki disease for which it is likened. And thus, this sets up the discussion of the various similarities and differences of these two clinical entities (Esteve-Sole et al., 2021; Verdoni et al., 2021).
By definition, a multisystem inflammatory syndrome in children and Kawasaki disease have a lot of similarities; this is regarding the vast majority of the clinical manifestations and the target age group. While Kawasaki involves a much younger age group, MIS-C is seen to involve much older children even up to the age of 14 years; despite their closely similar presentations, some classes of MIS-C present with more severe presentations than Kawasaki disease (Verdoni et al., 2021). Their etiology also plays to the same tune with some similarities and notable differences. Kawasaki disease has been proposed as a vasculitis arising from exposure to an infectious agent in a child that is genetically susceptible to developing the disease (Ozen, 2005). In MIS-C, the causative agent is undoubtedly SARS-COV-2 infection in Covid 19.
The pathogenesis of these two disease entities is also interesting. The multisystem inflammatory syndrome has no truly identifiable underlying mechanism but it has been hypothesized that there could be an element of direct vascular infection by SARS-COV-2 or through downstream activation of immune mechanisms and cytokine cascades. Kawasaki Disease however has more established pathogenesis. It is characterized by immune system imbalances with a particular focus on cytokine activity. The immune complex deposition has been cited with the association of type III hypersensitivity as well (Esteve-Sole et al., 2021).
A strong link to changing cytokine profiles is common to both MIS-C and Kawasaki disease and it is hypothesized that the unique nature of their individual profiles is necessary for distinguishing the two diseases (Esteve-Sole et al., 2021). Firstly, with regard to cytokine levels, MIS-C patients can be subdivided into 2 groups: 1 similar to Kawasaki Disease in terms of
clinical and cytokine profiles (described as Class 3) and 2 which is true or classic MIS-C, (described as Class 1) (Esteve-Sole et al., 2021; Godfred-Cato et al., 2020).
Cytokines produced have been shown to be IFN-γ–related and enriched win IL-1 and inflammatory monocyte pathways. These pathway involvements suggest that the role of the cytokines produced is principal in the inflammation seen in the disease manifestation of both MIS-C and Kawasaki diseases (Esteve-Sole et al., 2021; Verdoni et al., 2021). Although increasing levels of cytokines are seen in the circulation of covid patients at large, this is quite mild and not comparable to MIS-C patients who display an increase in inflammatory cytokines including IL-10, IL-6, IL-8, CXCL10, MIP-1a, MIP-1ß, TNF-a, and IL-17-a. circulating cytokine levels also increase in Kawasaki disease and especially seen with IL-17, which only rises moderately in MIS-C. Macrophage activation syndrome is also suspected in the more advanced disease of MIS-Cplus characterized by the marked increase in circulating levels of IFN-γ, IL-18, and IP-10 (Esteve-Sole et al., 2021).
The findings characterizing MIS-C and Kawasaki disease may be important is current management of covid 19 pediatric patients. By distinguishing the two entities one can more accurately make a timely diagnosis and institute lifesaving treatment. Additionally, it could be useful for the development of targeted therapy to optimize patient management and, in the long run, reduce mortality of covid 19 pediatric patients (Esteve-Sole et al., 2021; Verdoni et al., 2021).