Chronic Obstructive Pulmonary Disease
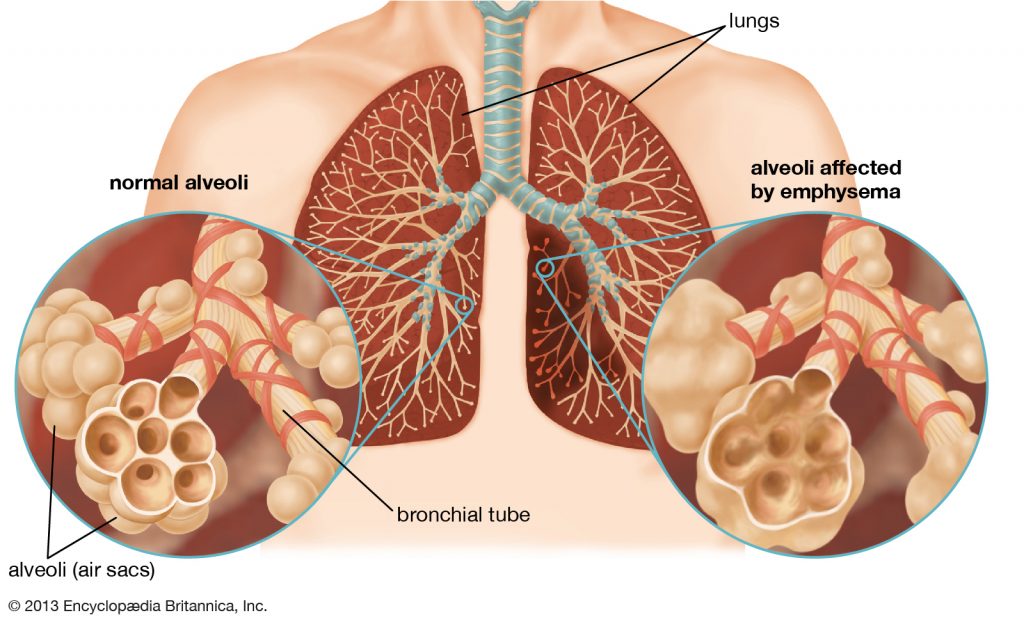
Chronic illnesses are the leading cause of deaths and disabilities in the world. The diseases, therefore, require the use of integrative management to contain them. Patients suffering from COPD in particular need to be involved in the health care process. In many patients, the disease can lead to impaired functionality, increased mortality rates, and reduced quality of life. For example, Mrs. Smith is a 65-year-old woman with breathing difficulties, dry cough, sputum production, and wheezing. Before the diagnosis of the Chronic Obstructive Pulmonary Disease, Mrs. Smith suffered a rib fracture as a result of a car accident in 2016. She has also been admitted twice for emphysema due to excessive smoking and exposure to harmful gases in the atmosphere.
Mrs. Smith lives adjacent to a manufacturing company; hence, the toxins released from the industry contributes to her respiratory problems. Apart from the constant coughs and wheezing, she has been in good state of health until this week when she complained of chest congestion and shortness of breath as she climbed the stairs. She also experienced swelling of the legs and low energy levels which prompted her to seek medical attention.
The current plan of care for Mrs. Smith involves the auscultation of the breathing sounds, assessment of the noting rate and the inspiratory, and the expiratory ratio. It also involves the use of the American Thoracic Society’s “Grade of Breathlessness Scale” to ascertain the breathing difficulties (Sundh & Ekström, 2016). To make her more comfortable, she is to sit on the edge of the bed. Additionally, she is required to raise the head side of the bed. She has also been put on therapy to stop smoking to improve her health. Mrs. Smith is also advised to relocate to a less polluted area to ease the chest congestion and help her recover from the COPD. Finally, she is encouraged to increase her fluid intake per day will, and chest physiotherapy will be applied.
The clinic is privately owned and run by six General Practitioners. There are five more employed GPs; hence, the total number is 11. There are 14 registered nurses; one mobile nurse, two respiratory nurses, and two occupational health nurses. The support staff includes the dietetic assistant, two physiotherapy assistants, one radiography and imaging support assistant. They also include one nutritionist, one social worker, one phlebotomist, and two theater support workers.
The clinic has a patient roll of 6,000, mainly the middle class and the upper class. A majority of the patients are from 23 years to over 65 years with both long term and short term conditions and several comorbidities. Underage patients are rarely admitted in the hospital as most of them utilize the outpatient facilities. The clinic provides general medical services, including plastering, radiology services, women’s health, podiatry, and immunizations. The common diagnoses seen are asthma, hypertension, acute maxillary sinusitis, acute bronchitis, myositis, emphysema, osteoarthritis, and patients who require general medical examinations.
The best model proposed for this setup is the COPDnet integrated care model. According to Koolen et al. (2018), the model serves as a blueprint for the establishment of the provision of care for COPD patients in health care settings. It provides a distinction of seven phases; “a screening phase, a project management phase, a diagnostic phase (baseline measurements, mapping existing pathways), a design and plan phase (development of care pathway), an implementation phase, an evaluation phase, and a continuous follow-up phase (making it clinical routine and ongoing review)” (p.2226).
The model involves the use of diagnostics in the secondary care setup and the use of the nonmedical intervention in the provision of primary care. It also entails rehabilitation in a tertiary care setup. The elements in the COPDnet integrated care model include “self-management support, decision support, delivery system design, and clinical information systems.” (Klooner et al., 2018). The model is based on principles such as individualized care plan for different patients. The physicians achieve this by assessing the determinants of the disease carried out near the home of the patient. It also fosters behavior change by introducing self-management for the patients.
The model will be useful for patients with respiratory problems as it encourages self-management skills among patients. These skills include behavior changes such as reduced smoking, increased fluid intake, and reduction of respiratory pollutants such as feather pillows (Effing et al., 2016). The COPDnet integrated care model offers this support by assessing the knowledge of the patients through interviews and Capabilities Opportunities Motivation-Behavior (COM-B) model to identify the determinants of human behavior (Koolen et al., 2018). It also involves shared decision making, which allows the patients to choose and explore their preferences regarding lifestyle change. Finally, the patient is allowed to construct an individual care plan which will later be developed into preferred treatment options.
Additionally, the model will be useful as it provides additional diagnostics, the burden of disease classification, and personalized interventions (Koolen et al., 2018). The extra diagnostics determine the traits of individual patients hence providing personalized care which facilitates their recovery. The classification of the burden of disease enables the nurses to allocate the patients with the proper care setting. It includes referral to a primary, secondary, or tertiary care setting depending on the severity of the infections. According to Ekström, Sundh, and Larsson (2016), the use of Patient-Reported Outcome Measurements (PROMs) also facilitate the delivery of care by providing follow up on the patient diagnosis. The patient is, therefore, monitored for a period leading to a full recovery.
The delivery of the care in the COPDnet model also facilitates its effectiveness. It achieves this through the systematic feedback gathered from Patient-Reported Outcome Measurements. The presentations and discussions carried out between the pulmonologist, respiratory nurse, and the psychologist helps in the decision-making process in the hospitals (Klooner et al., 2018). The outcomes of these discussions favor the patient health status, the frequency of the diagnosis, and individualized care plans. In so doing, the patients receive quality care and improve their recovery process. The model also provides for education and training sessions for the health care providers to facilitate the delivery of care.
Finally, the model encourages the use of Electronic Health Records (EHR). The data storage method allows for easy access to patient information and history. With this information, the General Practitioner can evaluate individual health status, which aids in the decision-making process regarding the patient. The digitization of the model improves its efficiency and facilitates the sharing of information between health care providers. Generally, the model caters for the needs of the patient by facilitating the access to information, the provision of disease management option, training sessions for the practitioners, and monitoring of the patients through routine checkups.
The model will fit in the clinical setting as most of the diagnosis involves respiratory issues. The COPD patients, for instance, require a patient-centered approach to facilitate wellness. The individualization provided by the model offers information about the treatment and the expected outcomes hence improving the recovery. The approach fosters the direct involvement of the caregivers and the patients to better health.
To facilitate the implementation of the COPDnet integrated care model, the hospital will need to provide more resources for its application. The model includes discussions, education, and training. At the moment, the clinic does not have facilities such as conference rooms and projectors, which will facilitate the training. Investing in such facilities will, therefore, enhance the implementation of the model. Additionally, the clinic will need to employ more physiotherapists, dieticians, and occupational therapists to facilitate the nonmedical interventions for the patients. The model provides for personalized interventions to facilitate the recovery process. The interventions require the help of support staff to ensure that patients adopt good self-management practices to ease their recovery from COPD and other respiratory diseases.
The clinic also needs to improve its information systems to allow secure storage and retrieval of patient data. The effectiveness of the model is dependent on the ability to store critical clinical data of the patients during diagnosis. Improving the clinical information systems also eases the follow up on the patients. Easy access to information enhances the delivery of care and improves communication between health care providers.
In conclusion, the COPDnet integrated care model is designed based on the insights of the effective delivery of care for patients. The applications of the principles of the model allow health care providers to focus on the patient. Its feasibility in use in health care setups is based on the ease of implementation, the benefits to the patients, and the reduced cost of care.