Decorticate and Decerebrate Posturing
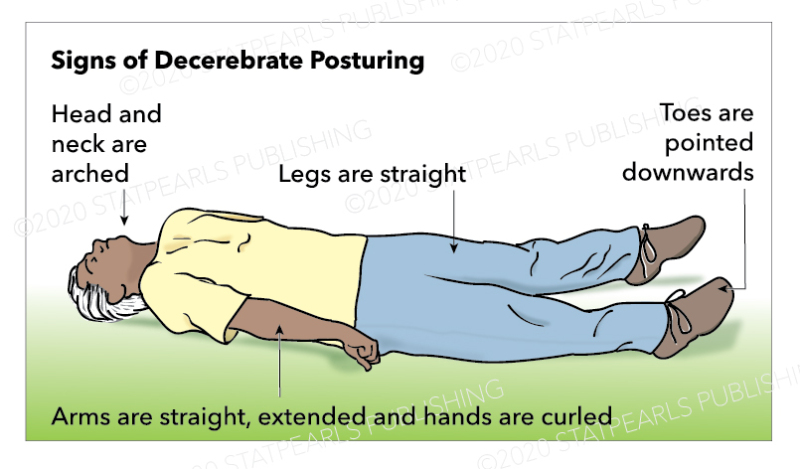
Decorticate posturing is an abnormal posture. A person becomes stiff with arms bent, fists clenched, and legs held out straight. The arms bend towards the body, fingers and wrists bend and are held on the chest. It indicates damage to the nerve pathway in the midbrain. Decorticate posturing is common in severe brain damage. In decerebrate postures, the hands and legs are usually straightened, the toes point downwards, and the neck and head are positioned backward. Muscles are tight and rigid. It can happen on one or either side or just the arms. Decerebrate posture is abnormal posturing indicating brain damage (Ignatavicius and Workman, 2013).
CT scan, MRI, PET, and Lumbar Puncture (Spinal tap).
CT scan is an imagining that combines x-rays and computers to bring out pictures of patients’ body organs, soft tissues, and bones. It produces more details than a normal x-ray. It can image almost all body areas and is used to diagnose illness or injury and plan medical or surgical treatment. Doctors recommend CT scans to; locate a tumor or clot, detect internal injuries, guide various surgical procedures, and diagnose certain disorders of the muscles or bone.
MRI is a non-invasive procedure with no pain that utilizes a strong magnetic field and radio waves to form images of tissues and organs in the body. It uses ionizing radiation, which is harmless to the body. It can be used to; detect spinal cord and brain abnormalities, tumor and cysts of the body, abnormalities of the joints, and certain heart problems (Ignatavicius et al., 2013). Little preparation is required for the patient before an MRI.
Lumbar puncture or spinal tap is done on a patient lower back on the lumbar region. A special needle is punctured between two lumbar bones to remove fluid from the procedure’s cerebral spine. The spinal-fluid surrounds the brain and spinal cord to prevent it from injuries. A spinal tap can be used to detect meningitis, bleeding in the brain, central nervous system disorders, and brain and spinal cord cancers. A spinal tap can also be used to inject anesthesia or chemo-therapy medication into the cerebral spinal fluid. It can also be done to; measure cerebral spinal fluid pressure and collect cerebral spinal fluid for analysis to detect any infections. It is a safe procedure but may also have certain risks like; headaches after the procedure, back pain or discomfort, and bleeding (Ignatavicius et al., 2013).
Symptoms and treatment of Migraine headaches.
Migraine headache is normally on one side of the head; it can cause intense throbbing pain or a pulsing sensation. Nausea, vomiting, and intense sensitivity to light and sound frequently accompany it. It might last for hours or days, and the pain can be so intense that it interferes with everyday activities. In some individuals, before the headache, they may experience aura. Tingling on one side of the face or leg, trouble talking, light flashes can be part of the aura. Symptoms of migraines progress in four stages. Prodrome stage symptoms; stiffness of the neck, increased urination, mood changes, and frequent yawning (Ignatavicius et al., 2013). Aura stage; vision loss, difficulty speaking, hearing noises, jerking, and weakness on the face. Attack stage symptoms; throbbing pains, nausea and vomiting, and light sensitivity. Post-drome stage symptoms; confusion, a patient may feel drained, and sudden head movement may cause severe pain.
There are risk factors related to migraines; family history of migraines, sleep disorders, depression, and hormonal changes; it is more common in females than males. There is no treatment for migraines, but medication is used to control the counter painkillers’ symptoms like ibuprofen, naproxen, and acetaminophen. Patients can also use cold packs, stay in a quiet, dark room, and nap when necessary (Ignatavicius et al., 2013).
Seizures, clinical manifestations, treatments, and nursing interventions.
Seizures are uncontrolled electrical disturbances in the brain. It can trigger changes in attitude, gestures or emotions, and levels of awareness. Most seizures last for 30 seconds to two minutes. Seizures that last more than five minutes are treated as medical emergencies. In most instances, the causes of seizures are unknown. People with recurring seizures can be considered epileptic. There are three types of seizures; tonic, clonic, and tonic-clonic seizures. The commonest cause of seizures is epilepsy.
The other causes of seizures are; brain tumors, head injury, high fevers, low sodium levels in blood, alcohol abuse, and some medications. Clinical manifestations of seizures include; confusion, jerking uncontrollable movements, loss of consciousness, and a patient may be unaware of what is happening, emotional symptoms such as fear and anxiety. Treatment includes; anti-epileptics (sodium valproate, carbamazepine, and lamotrigine), surgery to remove tumors causing the seizures, ketogenic diets to control seizures, and vagus nerve stimulator (it is placed under the skin on the chest and it helps prevent seizures) (Ignatavicius et al., 2013).
Nursing interventions in seizures management include; monitoring seizure events, ensuring a safe environment for patients, providing oxygen when a patient becomes cyanotic, placing patients on their side when a seizure occurs, protecting patients head during a seizure, not restraining patient during a seizure, placing patients’ beds low to prevent injury, teaching patients how to control stress, advise patients to avoid alcohol as it interferes with seizures medication and maintaining airway until the seizure goes away (Ignatavicius et al., 2013).
Meningitis clinical manifestations, treatments, and nursing interventions.
Meningitis is an inflammation of the meninges. Meninges cover the spinal cord and brain. Viral and bacterial infections cause it. Meningitis infection can improve with treatment within weeks, and in some cases, it can be life-threatening. Meningitis symptoms include; neck stiffness, fever of sudden onset, seizures, confusion, light sensitivity, lack of appetite, severe headache, difficulty walking, nausea, and vomiting. If not, well-managed meningitis can lead to complications, damage to the brain, hearing loss, vision loss, and hydrocephalus. Lumbar puncture, blood culture, MRI, and CT of the brain can diagnose meningitis (Ignatavicius et al., 2013).
Medication depends on the type of meningitis. Medication includes IV antibiotics, corticosteroids; diazepam can be used to control seizures, IV fluids to prevent dehydration, and oxygen in breathing difficulty. Several nursing interventions can be considered, like; monitoring vital signs, seizure activity, and signs of increasing ICP. Additionally, monitoring meningeal irritation signs, ensure the patient gets enough fluids, and administering drugs as prescribed should be done. Furthermore, maintaining stool and urine precautions with viral meningitis and performing cranial nerve assessment is vital (Ignatavicius et al., 2013).
Alzheimer’s disease, clinical manifestations, stages, and nursing management.
Alzheimer’s disease is a condition that causes brain cells to wear out and die. It is the commonest cause of dementia. It tends to develop slowly and gets worse over the years. The disease normally affects memory, judgment, thinking, and personality. Alzheimer’s disease occurs in three stages early, middle, and late stages (Ignatavicius et al., 2013). In the early stage, patients might function independently. They can work, engage in social activities, and carry out their daily routine. Patients may have memory lapses; they can forget familiar words, places, or objects.
An individual may fail to recognize the symptoms in this stage, but people close to those affected, and doctors may recognize the symptoms. Patients may have difficulty in; coming up with the correct words, remembering people’s names, performing tasks at work, and organizing or planning things. The middle stage can last for many years, and patients need more care and better management.
Dementia symptoms are more in the middle stage. Symptoms vary depending on individuals. Symptoms may include; forgetting events or personal history, feeling withdrawn and moody, being confused about where they are or what they are doing, difficulty controlling the bladder, changes in sleep patterns, and being unable to recall their personal information. Patients can participate in daily activities but with help. In the late stages, the symptoms are very severe. In this stage, patients are not able to communicate, and their memory becomes worse. Patients may be unable to respond to their environment (Ignatavicius et al., 2013). At this severe stage, patients may; not be able to communicate,they become more prone to infections, have a change in physical abilities, require daily personal care, and they may not be aware of the surroundings.
Nursing management required includes; providing psychological support to patients and family, giving patient medications as prescribed, and protecting patients from accidents. Again it should be ensured that the patient gets involved in some physical activities and can carry out some tasks independently. Additionally, the patient should be helped to communicate effectively with family members, ensuring they are clean, getting enough rest, proper nutrition, and sufficient fluids (Ignatavicius et al., 2013).