Medication-Assisted Treatment (MAT) to Treat Substance Use Disorders (SUDs)
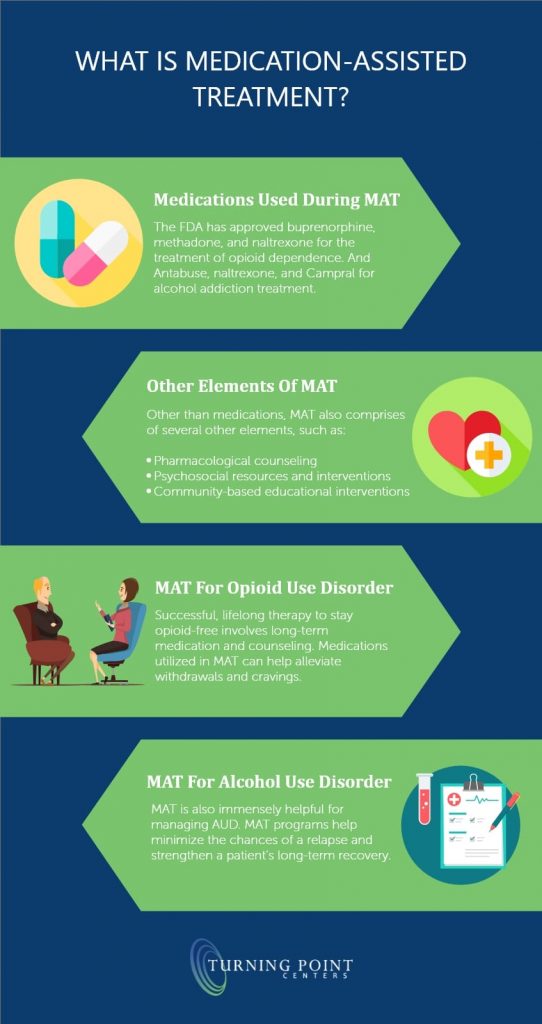
Substance use disorders (SUDs) caused by drug abuse affect an individual’s brain and behavior, decreasing their quality of life and health. Medication-assisted treatment (MAT) is among the most effective approaches to addressing SUD. It refers to using a combination of medicine, counseling, and behavior therapies to address SUDs and avert opioid overdose (Dowell et al., 2016). Methadone, and buprenorphine, among others, are utilized in heroin, morphine, and other opioid-related addictions (Andraka-christou, 2016). A common misunderstanding associated with MAT includes the perception that the approach substitutes one drug for another. This false perception results from the lack of knowledge regarding how the MAT approach works. However, the approach utilizes medications approved by the Food and Drug Administration (FDA), and the program comprises clinically driven and customized strategies to meet a specific client’s needs (WHO, 2009). MATs medication helps relieve patients’ withdrawal symptoms, including psychological cravings that result in the body’s chemical imbalances (Andraka-christou, 2016). Thus, MAT programs present SUD individuals with a safe and controlled therapy level to overcome the condition. Through learning MAT, I have realized that many people view individuals suffering from SAD as hopeless, a “lost cause,” or insane, but most SUDs patients do not comprehend the available resources to help them through the path to overcome the problem.
The CDC guidelines recommend nonopioid treatments and nonpharmacological approaches as the most complementary therapies to promote safety and care quality for palliative, end-of-life, and active cancer patients. Opioids should not be considered the first therapy line as they present significant risks to overdose or escalate the opioid use disorder (CDC, 2014). Caregivers should consider opioid therapy where expected benefits are anticipated to outweigh patients’ potential risks (Dowell et al., 2016). The current “crackdown” on opioids prescription in America presents unintended consequences. Advocating for fewer and shorter opioid prescription periods increases patients suffering, especially to patients with cancer, palliative, and patients at the end-of-life. Besides, the “crackdown” results in withdrawal tapering effects, causing people to seek street drugs such as heroin (Karlin-Smith & Ehley, 2018). Also, reports indicate that suicides among people left with uncontrolled pain have increased since the opioid prescription crackdown (WHO, 2009). These consequences present further challenges of dealing with the opioid pandemic in the country.
Weaning patients off prescribed opioids should be a gradual and cooperative process for the therapist and the patients, but not an ultimatum that creates a sense of abandonment among patients (Karlin-Smith & Ehley, 2018). It is relatively difficult to put patients off opioids, especially in chronic pain cases. Nurses should collaborate with social workers, psychologists, among others, to address anxiety and the need to establish other alternatives to opioid prescriptions (Dowell et al., 2016). Studies indicate that putting patients off opioids increases their quality of life (Karlin-Smith & Ehley, 2018). Thus, nurses have the responsibilities of monitoring patients experiencing opioid withdrawal symptoms, dispensing medications as directed by the physician, counseling, and engage them in other activities that disrupt their opioid cravings (Moore, 2020). Furthermore, since patients’ withdrawal may result in anxiousness, fear, and violence, nurses should offer accurate and realistic information about the withdrawal to alleviate fear ad anxiety (CDC, 2014). However, applying these strategies may prove challenging as patients experiencing withdrawal symptoms portray violence and disruptive behavior, making them difficult to manage.
Sober homes allow drug addicts to focus on their recovery by engaging in healthy activities while processing numbing feelings and other challenges. Stress, self-denial, judgment from society, alienation, and a sense of guilt significantly contribute to a relapse. Sober homes promote a personal sense of belonging, provides them with an opportunity to live and interact with people experiencing similar challenges as they understand and relate to them (Possomato-Vieira, José S. and Khalil, 2016). Moreover, sober homes promote personal responsibilities to self and others, improve communication skills, and help individuals set healthy boundaries. Sober homes eliminate the stigmatization associated with rehabilitation centers while providing a safe and conducive environment to enhance an individual’s journey towards sobriety (Possomato-Vieira, José S. and Khalil, 2016). I would look for some essential aspects in a sober home, including recovery support services, accountability, education, employment placement services, safety, quality accommodation, and cultural competencies (Possomato-Vieira, José S. and Khalil, 2016). Such aspects are essential in enhancing promoting a patients’ journey towards recovery and sobriety.