Comprehensive Discussion On A Person-Centred Approach To Caring For A Person In End Of Life
Introduction
This assignment provides an assessment of the knowledge gained about delivering person-centred care to individuals in their end of life. The paper includes the definition of palliative care, the history of palliative care, and its importance in the current society. Principles and philosophies of palliative care are also described. The holistic needs of a client in their end of life will also be addressed, including how a clients’ needs for safety, dignity, respect, and comfort can be met in end-of-life care are described. Finally, the importance of patient-centred care and communication in end-of-life care will be provided.
What is Palliative Care
History of Palliative Care
Palliative care is a relatively new concept that has evolved significantly over the last few years. The historical roots of palliative care extend back to ancient times, and it began with a focus on caring for the dying. The initial concepts of modern hospice care were articulated in the 1950s by Dr. Cicely Saunders, and these concepts were based on careful observations of dying patients. In the 1960s, Elisabeth Kübler-Ross, a United States psychiatrist, challenged the failure of the healthcare system to treat patients in their end of life with respect, openness, and honest communication. The care for dying patients was later revolutionized and humanized through her groundbreaking book titled On Death and Dying (Loscalzo, 2008).
The term palliative care was initially coined by Dr. Balfour Mount in 1974, who later included Dr. Saunders innovations and concepts into academic teaching in hospitals. In Ireland, palliative care services are currently considered as a medical specialty. Hospice in Ireland originated in the 19th century when Our Lady’s Hospice in Dublin and St. Patrick’s in Cork by the Sisters of Charity were established. In the 1980s, the modern palliative care movement in Ireland began, which has been an advocate and catalyst for the development of palliative services in Ireland. In 1990, the Irish Association for Palliative Care was established. The organization promoted the development of palliative care specialty, and in 1995, palliative medicine was recognized as a medical specialty (Loscalzo, 2008).
The Need of Palliative Care in Today’s Society
Palliative care is required for a wide range of medical conditions. Palliative care is vital is relevant in the current society because it is concerned with suffering, care needs, and the quality of life of people at the end of their lives. Currently, lifestyle changes and other factors have increased the prevalence of chronic conditions, which increase the need for palliative care services. Palliative care enhances the quality of life of patients experiencing life-threatening illnesses and that of their families. Palliative care also improves the quality of life of caregivers. According to the World Health Organisation (WHO) (2018), 40 million people need palliative care every year, and approximately 78% of these live in low- and middle-income countries. Despite these statistics, globally, only 14% of the patients who need palliative care receive it. Most patients who need palliative care live with chronic conditions such as cardiovascular diseases (38.5%), diabetes (4.6%), kidney failure, chronic liver disease, rheumatoid arthritis, cancer (34%), and chronic respiratory disease (WHO, 2018). Various research studies have provided evidence of the benefits of palliative care in improving patient outcomes (Institute of Medicine [IOM], 2015).
End-of-life Care Organisations in Ireland
The Irish Hospice Foundation is an organisation in Ireland that provides end-of-life and bereavement care. The organisation offers services such as Nurses for Night Care and Bereavement Support Line. The organization also provides education and training in end-of-life and bereavement care. Additionally, the Therese Brady Library is available within the organisation, and it is dedicated to death, bereavement, and dying (Irish Hospice Foundation, 2019). All Ireland Institute of Hospice and Palliative Care (AIIHPC) is situated in Dublin, Ireland, and is a leading organization that influences palliative care nationally and internationally. The organization advances research education and practice for the improvement of palliative care experience for patients living with life-limiting conditions (Wescott, n.d.).
Principles and Philosophy
Definition of Palliative Care
According to WHO, palliative care is an approach that results in improvement of quality of life of patients and families facing the problems associated with life-threatening illnesses through the prevention and alleviation of suffering by identifying, assessing, and treating pain as well as other physical, psychosocial and spiritual problems (Al-Mahrezi and Al-Mandhari, 2016, pg. 161).
Principles and Philosophy of Palliative Care
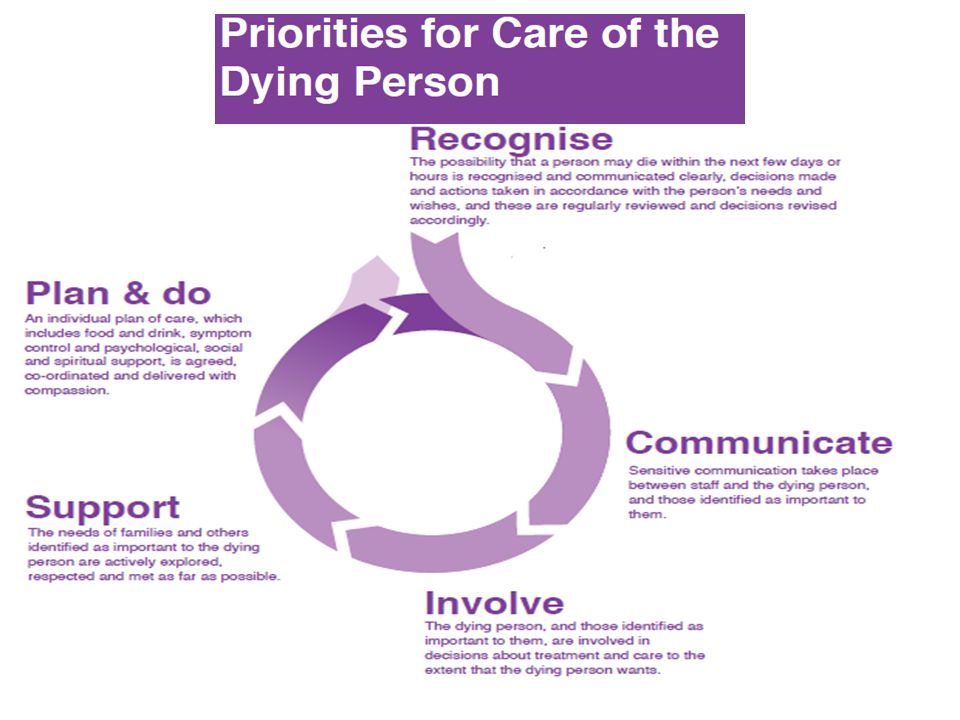
A central principle of palliative care is that it focuses on relieving pain, suffering, and distressing symptoms. Palliative care upholds that life is a normal dying process and hence does not intend to hasten or postpone death. Additionally, palliative care integrates spiritual and psychological aspects in palliative. Another principle of palliative care is that it offers a support system to help patients live a meaningful life until death and to help their families cope during the patients’ illnesses and in their bereavement. Palliative care utilizes a team approach to address the needs of the patient. Finally, palliative care is applicable in the early course of an illness as it is combined with other therapies that focus on prolonging life and improving the quality of life. The philosophy of palliative care is that it is person-oriented, not concerned with life-prolongation, and not concerned with long-term disease remission. Palliative utilizes a multidisciplinary approach and is dedicated to the quality of life of the patient.
Person-Centred Care
Holistic Needs of Clients in End-of-life
Patients at the end of life have complex needs, including physical, social-emotional, spiritual, and psychological needs. Physical needs depend on the patient’s underlying illness. Often patients at the end of their life experience pain, nausea, vomiting, and breathlessness. To address biological needs, healthcare practitioners focus on symptom control through the use of opiates and complementary therapies. Individuals with life-limiting diseases may also feel distressed and anxious. The psychological needs of clients at the end of life also relate to the patient’s physical needs. For instance, if a patient’s underlying disease causes dyspnoea, the patient may become anxious, which may aggravate the problem. For such a patient, therefore, the use of medications or simple interventions such as the use of fans may help alleviate the anxiety. At the end of life, patients need to experience the connection of relationships in human life. Additionally, the therapeutic relationship is vital to maintain and involves shared decision-making between the healthcare providers and the client (Hackett, 2017, pg. 144). Two critical spiritual needs for patients in their end-of-life are ending disagreements with others when possible and finding meaning in one’s own life. Patients also have a need to know about their illnesses (Kennedy, 2016, pg. 44).
Meeting a Client’s Safety, Dignity, Respect, and Comfort
Safety for patients at the end of their life can be met by ensuring a multidisciplinary care approach characterized by effective communication is adopted. It is also crucial to identify the cause of anxiety, issues that cause most distress, and relationships that give hope. A client’s respect and dignity at the end of life can be upheld by implementing interventions such as enhancing social support, promoting independence, creating a respectful environment, assisting the patient with personal grooming, ensuring patient privacy, symptom control, and using a positive tone of care. Additionally, showing respect, compassion, and empathy encourages a sense of dignity. Patient dignity can also be promoted by encouraging life review (Kennedy, 2016, pg. 45). Symptoms control alleviates the patient’s pain, thus ensuring that the patient is comfortable.
Importance of Person-centred Care
Person-centred care (PCC) involves caring for an individual beyond their illness and personalising services that address the needs of the patient. It involves ensuring that the patient involved in decision-making and viewed as an individual capable of making personal health decisions. Patients with palliative care needs require support with their holistic needs, including physical, emotional, spiritual, and social needs. PCC ensures that the patient with a life-limiting illness drives the care provided. PCC improves care outcomes and enhances satisfaction with the care provided.
Communication
Importance of Communication End-of-life Care
Effective communication is especially vital for fostering relationships at the end of life. Stress and grief often catalyse conflicts among family members. Hence effective communication through open conversations reduces these conflicts (Hackett, 2017, pg. 144). Efficient communication ensures that’s staff members can identify the patient’s priorities and wishes. It also provides an opportunity for exploration of anxieties or gaps in understanding the situation. Through effective communication, healthcare professionals can reassure patients and their families, thereby alleviating anxiety and stress. Communication allows healthcare professionals to initiate, facilitate and respond to sensitive conversations. Additionally, effective communication ensures that a patient’s family members are well appraised of the patient’s condition, treatment, and care provided. More importantly, communication between interprofessional teams and at points of care transition ensures the best patient outcomes (Dunne, 2005).
Key Communication Strategies in End-of-life Care
Various communication strategies are applicable when communicating with patients nearing their end of life. These include the use of open-ended questions, the use of verbal and non-verbal expressions of empathy, and aligning the communication with the hopes of the patients and their loved ones (Archer, Latif and Faull, 2017). Open-ended questions promote a greater understanding, while the use of verbal and non-verbal empathy expressions encourages the patient to share more details about their life. It is essential to focus on what is acceptable to the patient, and in addition, the use of semi-structured plans results in viable conversations. Being direct, confidant, and calm can be comforting. Constantly reassuring the patient is critical.
Barriers to Effective Communication
Some barriers to effective communication include failure to allow adequate time for the patient and family members, discomfort with end-of-life conversations, lack of sufficient preparation, presentation of treatment prognosis in a biased manner, and lack of consensus among the healthcare team members (Schultz, 2019). The healthcare worker may also fear to upset the patient, cause more harm than good, say the wrong thing, and deal with patient’s emotional reactions.
Conclusion and Evaluation
Findings and Recommendations
Palliative care is vital in alleviating pain and suffering among patients nearing the end of life. The concept of palliative care was introduced in the 19th and 20th centuries, and currently, the specialty has gained recognition as a medical specialty both nationally and internationally. A multidisciplinary team approach is vital when delivering palliative care, as it ensures the development and implementation of comprehensive care plans. This care approach also facilitates care coordination, quality improvements, and appropriate pain management. Effective communication and the delivery of PCC are vital in improving the health outcomes of palliative care clients. WHO asserts that those who need palliative care do not receive it. Development of core components of quality end-of-life care would be helpful in ensuring that people nearing the end of life receive quality healthcare services. Some of these components include management of emotional distress, family caregiver support, attention to the patient’s spiritual and religious needs, addressing the patient’s social needs, and referral to expert palliative care services. Given the cost-effectiveness of palliative care, health care systems policies need to integrate palliative care services in all levels of the healthcare system.
Reflection on Knowledge Gained
Life-limiting illnesses impact patient’s daily life; hence palliative care has an influence on everyone, and as a healthcare worker, gaining knowledge and skills required to care for patients with life-limiting illnesses is crucial. The main focus of palliative care is helping patients by alleviating their pain and suffering, regardless of the patient’s prognosis or disease stage. The purpose is to improve the quality of life of patients and their families.