A.C. 1.1 Homeostasis And The Role Of The Nervous System And Endocrine System
Despite ongoing external and internal changes, optimal circumstances for cells can be maintained through the dynamic processes of homeostasis. Every human body is involved, with the endocrine, neurological, respiratory, and urinary systems making particular contributions. Whenever an imbalance arises, regulatory systems activate to restore ideal conditions. Typically, this is achieved through negative feedback, in which a deviation from the expected standard is detected and causes adjustments that restore the appropriate levels. These systems must persevere for survival and adjust to environmental changes to evolve.
The central nervous systems and the endocrine systems are the core control systems for homeostatic control maintenance. A collection of glands in the endocrine system secrete hormones(MASAKI, 2018). The nervous system can detect variances from the body’s homeostasis and communicates with the affected organ to instruct it to correct the issue. It reinstates the required equilibrium in a reasonable amount of time
The organs and organ systems of the mammalian body function like well-oiled machinery controlled by the endocrine and neurological systems. The organ systems together supply the body’s cells with all the necessary substances and remove their wastes. In addition, they maintain optimal amounts of temperature, acidity, and other variables to sustain living activities. Although the nervous system can be partially controlled voluntarily, both operate primarily instantaneously. The management and maintenance of blood glucose levels by the endocrine system are instances of homeostatic regulation(Whitney et al., 2020). Glucagon and insulin are pancreatic hormones that regulate blood sugar levels. Following digestion, glucose levels rise in the blood. In reaction, pancreas cells secrete insulin, allowing cells to absorb sugar and store it in the muscles and the liver. Insulin efficiently normalizes glucose levels.
A.C. 1.2 Reflex Action
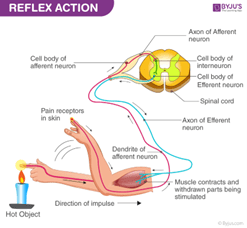
A simple form of stress is a reflex action when a stimulus prompts an immediate response. A reflex is an unanticipated, involuntary response to a stimulus. Additionally, it is a crucial element of the well-known survival instinct. Most of our common responses are a product of our calm, collected knowledge of caution (Whitney et al., 2020). The sudden hand withdrawal from a hot object is a prime example of a reflex response. Subtly, it is connected to instincts. One thing to remember is that every one of us has a unique intuition predicated on our prior knowledge and experiences. A reflex is an instinct-driven reaction. Occasionally, it’s difficult to recognize whether something is hot or not. In other words, reflex and intuition are not the same things.
Figure 1: Reflex Action
The above diagram depicts the brain pathway that controls a reflex. It clearly shows the path taken when a stimulus happens and how the reaction occurs. Two types of neurons dominate the receptor’s direction and the effects (Porte, Baskin, and Schwartz, 2019). When the receptor notices the stimulus or a sudden change in the environment, instinct once more enters the picture. A sensory organ provides stimulation. The relay neuron subsequently relays the message to the motor neuron when the sensory neuron has finished transmitting its signal. The effector receives a call from the motor neuron, which prompts an immediate action, like moving the hand away.
A. C. 1.3 Action Potential Generation And Propagation Of Nerve Impulse
The neuron’s body generates a nerve impulse, which is then sent through its axon. The intensity of the nerve impulse is unaffected by propagation; thus, the target tissue receives the same impulse regardless of its proximity to the neuronal body. On the cell membrane, in just one place, the action potential is produced. Each next segment of the cell wall becomes depolarized as it moves down the membrane. This suggests that the neuronal membrane nearby generates a new action potential instead of the action potential moving. Ion channels adjust their structural characteristics in response to changes in the electrical field across the membranes (Porte, Baskin, and Schwartz, 2019). These structural reforms lead pores – channels – to open, allowing ions to flow down the electrochemical potential. Ion charge generates an electrical current, which rapidly changes the membrane potential with time- and voltage-dependent features. The resting potential represents the resting condition of the neuron, which is characterized by a net negative charge. Resting neuronal potential is around -70 millivolts (mV). The negative symbol denotes the cell’s negative charge relative to its environment. During depolarization, the charge changes from -70mV to +30mV. During repolarization, the charge changes from +30mV to -70mV.
The action potential refers to this quick, temporary shift in membrane potential. Action potentials carry information across neurons, cause muscle cell contractions, and cause exocytosis in secretory cells. On the other hand, synaptic transmission is the biological mechanism by which a neuron communicates with a target cell via a synapse. The delayed closure of sodium channels and the reopening of voltage-gated k+ channels result in repolarization. As a result, the cell’s sodium permeability restores to normal. As the input of sodium ions diminishes, slow voltage-gated potassium channels open, enabling potassium ions to leave the cell. This ejection restores the cell’s negative local membrane potential. Depolarization, sometimes referred to as the rising phase, occurs when positively charged sodium ions enter a neuron through open voltage-gated sodium channels. The polarity of the membrane potential changes when additional sodium enters the cell. Throughout this change in polarity, the membrane produces a transient positive value. Certain potassium channels remain open whilst sodium channels are reset during hyperpolarization. During the period of high potassium permeability before potassium channel closure, an excess of potassium is expelled. This leads to hyperpolarization, as seen by a transient dip following the spike.
A.C.2.1 The Glands And The Endocrine System
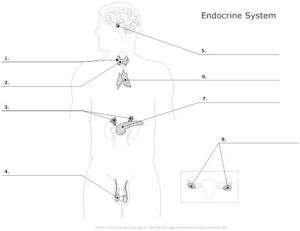
Figure 2: Glands and The Endocrine System
The endocrine system is a network of glands in the body that produce hormones that allow cells to communicate with one another. They are in charge of nearly every cell, organ, and function in the body.The endocrine system is made up of several glands. The brain contains the hypothalamus, pituitary gland, and pineal gland. The thyroid and parathyroid glands are located in the neck. The thymus is located between your lungs, the adrenal glands are located on top of your kidneys, and the pancreas is located behind the stomach. In the pelvic area are the ovaries for woman or testes men.
Different hormones are released by the glands that make up the hormonal system. Hormones play an important role in delivering messages from the glands to the target cell. Hormones are molecules that the endocrine system utilizes to communicate with organs and tissues all over the body. Hormones move via the circulation to their target organ or muscle, which possesses receptors that identify and react to the hormone.
A.C 2.2 The Mode Of Action Of Steroid Hormone And Mode Of Action Of Peptide Hormone
Steroid proteins influence metabolism, whereas peptide hormones influence membrane permeability. The action mechanisms of peptides and steroids are opposite. Evaluation of steroid hormones is generally based on the activation of genes and the creation of enzymes, which modify cellular activity. In contrast, protein enzymes act on peptide hormones’ primary mechanism of action by activating messengers. Steroid hormones have little effect on protein synthesis, but peptide hormones affect protein activity in the cell. Because of their fat solubility, these lipids are easily absorbed in cells, where they connect with steroid hormone receptors (Jessen et al., 2017). The resulting steroid hormones are released into the bloodstream before binding to specific carrier proteins.
A.C. 2.3 Positive And Negative Feedback Regulations Involving Hormones
Biological systems that maintain equilibrium are feedback mechanisms. This occurs when the result of an occurrence or response modifies the organism’s reaction to that occurrence or response. Positive feedback increases the rate of change or output: the response outcome is magnified to make it happen faster (Davis, 2019). Negative feedback reduces change or production: a reaction’s product is lowered to return the system to a stable condition.
Blood calcium concentration regulation is an example of negative feedback. In reaction to a reduction in calcium levels, the parathyroid glands secrete more parathyroid hormone (Pimentel, Ganeshan, and Carvalheira, 2019). Several biological processes are mediated by positive feedback. Positive feedback occurs when a response to an occurrence enhances the likelihood that the occurrence will continue. A mother nursing her child is an example of positive feedback. While a baby is nursing, nerve signals from the nipple stimulate the pituitary gland to generate prolactin. In response, prolactin kindles the mammary glands to give out milk, causing the infant to nurse more frequently.
A.C 3.1 Temperature Regulation
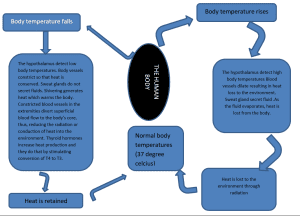
Thermoregulation is one of the most widely recognized examples of homeostasis. The average temperature is approximately 37 degrees Celsius. In spite of this, exposure to the outdoors, hormones, metabolic activity, and disease can all result in abnormally high or low-temperature levels. Negative feedback is utilized to maintain constant homeostasis in the body. The body cools itself through a mechanism called thermoregulation. The body is able to maintain its temperature within set limits even when the ambient temperature varies greatly.
Roughly 60 percent of the energy generated by cells during ATP production is used to maintain body temperature. Negative feedback is a mechanism for thermoregulation. As a thermostat, the hypothalamus regulates the body’s core temperature. The hypothalamus can launch a number of mechanisms to lower the body’s temperature if it rises too high. These include increased blood flow to the skin’s surface to facilitate thermal transfer and commencing perspiration to allow evaporative cooling on the skin’s surface (Davis, 2019). The hypothalamus can induce shivering to create heat if the body’s core temperature falls below the specified minimum. The body expends additional energy and generates additional heat.
Flowchart 1: Temperature Regulation
In conclusion, the endocrine system, similar to the central nervous system, is a regulating mechanism. Instead of electrical impulses, it makes and uses chemical messages known as hormones, which circulate in the blood and regulate organ and cell function. These and other homeostatic systems work continuously to preserve stability in the human body. However, occasionally the mechanisms fail. When this occurs, cells may not receive all the required nutrients, and harmful wastes may multiply in the body. The inability to restore equilibrium may result in sickness or even death.