Abstract
Schistosomiasis (Bilharziasis) is a disease caused by parasitic worms that live in certain freshwater snails and affect people in developing countries. Chronic Schistosomiasis with perianal fistula is an unusual presentation. We report the case of a 31-year-old Sudanese male who suffered from chronic anal discharge and was found to have a perianal fistula. He began empirically taking oral mesalamine three times daily, then underwent a colonoscopy to rule out Crohn’s disease and discovered Schistosoma eggs in a tissue biopsy. This case suggests that Schistosomiasis infection should be considered one of the causes of perianal fistula or abscess if the patient had traveled to endemic areas of Schistosomiasis in the past.
Keyword: Schistosomiasis, Intestine, Chronic perianal discharge/ fistula, Crohn’s disease, Endemic infection
Introduction
Schistosomiasis is an acute and chronic disease caused by parasitic worms of the genus Schistosoma. Schistosomiasis is widespread in the tropics and subtropics areas [1,2]. Most people who require treatment for Schistosomiasis live in Africa [1,2]. Most people have no symptoms when they are first infected. However, without treatment, Schistosomiasis can persist and become complicated. It commonly affects the intestine, liver, and genitourinary system and, less commonly, the brain and skin [1,2]. Patients with Schistosomiasis infection may have abdominal pain, enlarged liver, diarrhea, bloody stool, or bloody urine [1,2]. The diagnosis is made by detecting parasite eggs in the stool, or urine specimens also can detect Antibodies or antigens in blood or urine samples [1,2]. Praziquantel is the treatment of choice. It is a safe oral tablet and may prevent further complications [1,2]. A report by WHO, there have been several successful Schistosomiasis control programs such as access to safe water and hygiene education in the last 40 years in countries such as Brazil, China, Egypt, and the Middle East [1,2]. Intestinal Schistosomiasis may be confused with other disease states such as inflammatory bowel disease. Few data are documented about such cases but still uncommon and easily missed with other diagnoses, especially in developed countries [3-5].
We present a case of perianal fistula associated with Schistosomiasis in a gentleman who travels recently from A.L. Sudan.
Case Presentation
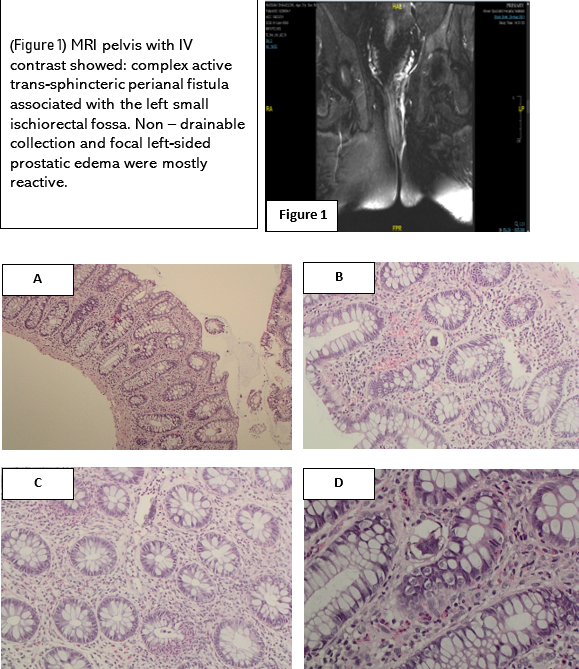
31-year-old Sudanese male residing in Saudi Arabia working as a driver, with no known medical illness. He complained of perianal pruritis associated with discharge for the last two years and was referred from general surgery clinic to gastroenterology clinic as a suspected case of Crohn’s disease and was prescribed mesalamine 1 gm orally three times daily as an empirical treatment for Crohn’s Disease. The patient denied a history of abdominal pain, change in bowel habits, and no mucus or bleeding per rectum—no history of fever, night sweat, or weight loss and no urinary symptoms. Regarding past medical and surgical history, he had a perianal abscess treated with incision and drainage three years ago. He had a history of inguinal hernia repair two years ago. Additionally, last year, he sought medical advice for a urinary tract infection subsided with antibiotics. On examination, the patient was vitally stable, and his general physical examination was unremarkable. There was a scar from the previous surgery at three o’clock with an external fistula opening on rectal examination. Basic laboratory investigations were unremarkable, including complete blood count, liver and renal panel, and urine. Complete stool analysis, including parasites, was negative. Magnetic resonance imaging (MRI) Pelvis with I.V contrast revealed perianal fistula (figure 1). Computed Tomographic (C.T.) enterography also showed perianal fistula. Colonoscopy was done, and biopsies were taken from different parts of the colon and sent for histopathology, which showed active colitis and proctitis with dense infiltration by eosinophils and multiple ova seen in the lamina propria of the Transverse colon, Descending colon, and Rectum (Figures A, B, C, D).
The diagnosis of Intestinal Schistosomiasis is made based on a histopathology report. The patient was advised to stop mesalamine, refer to an Infectious disease clinic and prescribe Praziquantel tablet, and planning to be followed with the Infectious disease and general surgery clinic for reevaluation, but unfortunately, he did not show up in the follow-up appointment.
|
Hematoxlyine and eosin staining of the pathology slides
Figures (A, B, C, D), (A) Magnification x4. It shows colonic mucosa with preserved crypt architecture. (B) Magnification x10. It shows lamina propria with increased number of eosinophils (>30/10 HPF) and calcified ova. (C) Magnification x20. It shows mixture of neutrophils and eosinophils with focal cryptitis and crypt abscess formation and another calcified ova. (D) Magnification x40. It shows calcified schistosoma egg. Type not specified. Biopsy was Negative for malignancy.
Discussion
In this case, a perianal fistula was suspicious for Crohn’s disease and not Schistosomiasis. It is a neglected infection that can be missed easily, especially in developed countries [5]. The two most common pathogens involved in intestinal infection are S. mansoni and S. japonicum. Many people tend to be asymptomatic. Only 5 to10% of patients with Schistosomiasis will be heavily infected [5-7]. Chronic infection may affect people and, in some cases, lead to complications such as liver fibrosis, kidney failure, or bladder cancer, and even death[5-7]. The clinical manifestation of chronic illness in the intestine are abdominal pain, diarrhea, constipation, or blood in the stool [6-7]. Symptoms of chronic intestinal Schistosomiasis are like other gastrointestinal diseases such as inflammatory bowel disease, peptic ulcer disease, or gastroenteritis. Therefore, many patients with Schistosoma are overlooked in other diagnoses and may lead to bowel wall ulceration, esophageal varices, and portal hypertension [6-7]. A careful travel and residence history is crucial in such cases. The diagnosis of Schistosomiasis is made by detecting ova in stool or urine specimens. Besides, serologic testing for Schistosoma antibody is part of the workup and follow-up. Basic laboratory tests are occasionally useful; for example, complete cell count (CBC) may show eosinophilia [6-7]. An invasive procedure such as upper and lower endoscopy is helpful when stool and urine samples are negative. Colon biopsy is more sensitive than stool microscopy in the setting of intestinal Schistosomiasis and may show granulomas surrounding eggs [6-7].
The treatment for all schistosome species is Praziquantel, and appropriate consultations to concern subspeciality depend on the complications but may include an infectious disease physician, urologist, gastroenterologist, or general surgery physician. Cure rates of 65-90% have been described after a single treatment with Praziquantel. After treatment, follow-up and reevaluation are required to prevent further complications [6-7]. Unfortunately, we cannot see such an outcome in our case as the patient did not show a follow-up appointment visit. Our patient is emigrating from an endemic area (Al Sudan). The presence of chronic anal fistula with a history of perianal abscess and unspecific findings by laboratory test and radiological imaging were considered further invasive interventions such as colonoscopy. The absence of eggs in stool or urine does not exclude Schistosomiasis, and our patient confirmed infection by the presence of ova and eosinophilia in colon biopsy. Finally, a good physician must look beyond the obvious and consider risk factors such as the patient’s country of origin and travel history to determine the possibility of an unusual illness.
In conclusion, perianal fistula is a rare complication of chronic Schistosomiasis that can mimic inflammatory bowel disease. Although rare, however, Schistosomiasis should be considered in the differential diagnosis of chronic anal fistula, especially in people coming from high-risk areas such as the patient in the case study. A biopsy is a useful diagnostic tool without demonstrative laboratory diagnostic tools. Treatment with Praziquantel may prevent further complications of this condition.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images.