Vaccination against Human Papillomavirus (HPV)
Introduction
- General
Human papillomavirus is one of the most common viral infections that are spread through contact. With more than 100 types, the virus leads in the list of the most commonly transmitted sexually transmitted diseases. About 40 of the varieties are spread from one person to another upon interacting with the mouth and genitals. The Centre for Disease Control and Prevention explains that the illness is fast becoming a menace globally for its association with various types of cancer (CDC, 2019). It is awful for its contribution to women’s cervical cancer. HPV 16 and 18 are the most prevalent types that demand special attention for their prevalence amongst the carcinogenic varieties of HPV. They are also associated with other malignancies that pose a health risk to various demographic groups. They are unpopular for causing both low and high-grade abnormalities of cells. Molecular tests for proteins, DNA, and DNA help determine the type that causes the malignant growth of cells as a result of HPV.
HPV is common amongst sexually active persons. The sexually transmitted illness spreads through anal or vaginal sex. In the US, a significant percentage of persons, especially the young populace, are sexually active. For this reason, the spread of HPV is a common occurrence. Around 79 million people in the United States have HPV. The worst issue about it is that a significant percentage of the people who are infected with the virus are not aware of their condition (Harder et al., 2018). For this reason, the virus keeps on spreading amongst sexually active persons without their knowledge. Health practitioners diagnose 14 million new cases each year. Most of the infections resulting from the virus go unnoticed, an issue that results in the fast spread of the virus. It is only through avoiding sexual engagements that a person can effectively prevent contracting the deadly virus. Parties within healthcare need to develop more effective ways of developing and administering human papillomavirus vaccination amongst the susceptible demographic groups.
Both men and women suffer from infections of HPV. In most cases, the infections affect the genitals of both sexes. More than 40 types of illness cause dangerous infections in the rectum, cervix, linings of vagina, anus, and the skin of the penis (Dunne, 2007). Although not necessary, the cancers that result from the infections affect the same areas. The back of the throat is also susceptible to cancer resulting from the same virus. The shocking fact about the virus is that it is not the only one transmitted through sexual engagements. The infections also spread from one person to another. In most cases, the infections are characterized by small skin growths in different parts of the human body. Also, brown and beige warts may appear on the body’s predominantly moist areas, such as the anus, mouth, and genitals.
Different types of viruses cause different infections and illnesses. Some types of the virus cause painless small warts on both the infected person’s face and fingers. Others cause flatter plantar, more painful, larger warts that grow on the feet’ bottom side. Other types of HPV infect the opening of the anus, cervix, and the skin covering the sex organ, including the vagina and penis (Dunne, 2007). These infections do not necessarily appear on everyone. For this reason, some people do not detect the infection—some people associate illnesses with other infections with similar signs and symptoms due to a lack of awareness. Ignorance, therefore, ensues amongst such people. Others experience the infections, but they disappear on their own after some time, usually two years. If sexually active, such people innocently incubate and spread the virus amongst their sexual partners. Such people stand a high risk of developing malignant cells that may eventually end in cancer.
- Scientific/ Mathematical Introduction
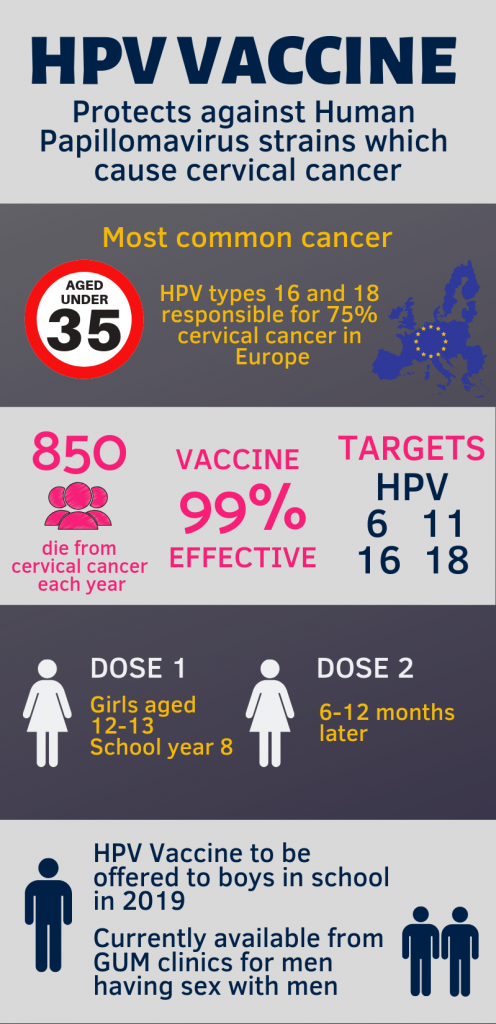
The illnesses that result from HPV consume considerable amounts of resources. It is especially bad amongst women since they are the ones who are usually affected by cervical cancer. Cervical cancer is the major cause of death among females around the globe. The Institute of Medicine states that types 16 and 18 of the HPV cause 70% cervical cancer (Chesson et al., 2008). It also attributes 80% of cases of anal cancer and 30% of vaginal and vulvar cancer to the two strains of the virus. The other two dangerous strains are type 6 and type 11 (Satterwhite et al., 2013). They are the major causes of anogenital warts. The costs involved are mainly used in the processes of screening and the treatment of genital warts and the resultant types of cancer. Various healthcare organizations are considering the possibility of reducing the prevalence of the illness through the development and administration of vaccines to women, especially in the ages of between 9-26 years. However, the vaccine is a cost that could be minimized if the vulnerable persons are well informed about the virus.
The costs of screening and treatment are high due to the need to cater to the affected persons with the utmost effectiveness. For example, the screening process requires resources to ensure acceptable test performance, adequate population coverage, and appropriate management of results that indicate the virus (Harder et al., 2018). A worse aspect of the costs is that the people who incur them are in their productive ages. The virus mainly affects sexually active individuals who are mainly young adults in their prime ages. The young people contribute significantly to the United States economy because they are produced compared to their older population. The virus reduces the productivity of people in their prime years, especially when they get cancer. Better use of the resources would have contributed significantly to their financial welfare. Instead, directing the finances to screening and treatment reduces the country’s economic status because it mainly relies on such people to enhance its economy.
- Cultural/Ethical Introduction
Among the main contentious issues regarding human papillomavirus is the matter of vaccines. Some people are concerned about the effectiveness of vaccination against human papillomavirus (Salwa & Al-Munim, 2018). The central issue surrounding the concern is that most vaccination programs do not offer adequate knowledge to the targeted persons. Most of the organizations that offer the vaccines do not adequately sensitize how they should take care of themselves and minimize sexual contact, amongst other related issues. Instead, the introduced programs neglect the other perspectives of the prevention against the related types of cancer. In Bangladesh, for example, a vaccination program was introduced in 2016 to assist in the demonstration of the vaccine (Salwa & Al-Munim, 2018). The program was initiated in the Gazipur district and eventually spread to cover the whole country. However, it faced a lot of criticism, owing to the failure of the persons administering it to offer significant information about HPV and cervical cancer to the persons to whom the virus was being administered.
Such situations raise concern regarding the ethicality of vaccination. One of the arguments within this issue is that some programs do not incorporate informed choice. Some people argue that it is important to adequately educate the targeted populace both for informed consent and the need to ensure that the persons involved are given the right level of freedom to choose whether or not to get vaccinated against the virus. Such programs should consider following a good plan that incorporates consent, information, and the ability to follow up on the programs’ possible adverse effects. Doing so can potentially eliminate protests against the persons and organizations involved in implementing the programs. More importantly, it can ensure that the persons targeted for vaccination are adequately informed regarding what is happening in the programs and know how to handle themselves as part of their prevention efforts against the virus and its resultant illnesses.
Scientific Perspective Inquiry
The economic burden or challenge of the cancers and precancers related to the HPV is substantial. The costs of managing and treating the disease are higher, especially the cost of vaccines in the United States. Scientists developed a vaccine that has helped treat the virus after seeing how much agony the virus was brought to people in the US and across the globe. The virus is meant to reduce the virus’s spread amongst the sexually active group in the country. HPV can be passed or spread through skin contact with an infected person. As a result, the virus aims to protect people from contracting the virus, leading to deep and serious health complications if not treated properly. HPV is the major cause of cervical cancer in most women and males around the United States and hence the need to develop the vaccine. However, the cost of purchasing the vaccine is high, and it snatches people their financial or economic freedom. Although most of the HPV-related infections disappear within a few days after infection, some stubborn infections fail to fade away even after treatment. Some after two or three years, some stubborn infections fail to fade away, resulting in serious health complications, including cancer.
Most anal, throat, and cervical cancers arise from the HPV. The cost of screening for cancer is high in the United States and most countries around the world. Some people have economic or financial strains, and this limits them from accessing appropriate screening on time. Early screening for cancer ensures a person starts medical treatment early, giving them better opportunities to recover from the virus. Early screening also reduces the cost of treatment because the disease is not severe, and few treatments and medications help correct the problem (Araldi et al., 2018). However, the cost of treating the disease at a severe phase due to lack of screening at the initial phases is higher. The cost of therapies and medication to treat cancer is higher, draining most people financially, especially if they do not have health care plans. Most people in the United States do not have healthcare plans due to the high cost. As a result, the population experiences challenges in paying the full cost of cancer treatment. Most families face or suffer from financial breakdowns because they used all the family resources and savings to cater to the cost of treating the virus.
Research conducted by the Centers for Disease Control and Prevention (CDC) indicates that most people in the United States suffering from HPV-related illnesses such as cancer are from the lower social class (CDC, 2019). Low socioeconomic status factors are the major cause of cancer arising from the HPV. Most people from low social-economic families cannot afford to pay for regular cancer screening in risk areas in the body, such as the throat or cervix. As a result, these people get infected with the HPV, and it spreads faster due to lack of treatment, thus resulting in cancer. Besides, most of these families cannot cover cancer treatment costs, including therapies and medications. Hence, they end up selling most of the family resources to take care of their patient. As a result, there is a relationship between social-economic status and cancer development from the HPV. Most families lose their breadwinner from cancer due to the HPV, thus exposing them to serious financial or economic breakdown.
The social conditions inhibiting the success of actions aimed at preventing and treating HPV illnesses are barely understood. Most of the scientists involved in research regarding human papillomavirus are inclined to research the development of more effective vaccines and treatment methods (Intemann & de Melo-Martín, 2010). They resort to neglecting the social conditions that would have otherwise served the most affected populations to gain from the research universally. Scientists have a crucial role in making the activities of prevention and treatment successful. However, a significant number of limitations deter them from being completely effective in so doing. Having to consider the social values involved in the development and application of HPV vaccines, for example, affects their effectiveness in ensuring effectiveness in their work.
Mathematical/Analytical Perspective
The need to analyze human papillomavirus arises from the extent of its effects. In the US, the virus affects about 70 million people. Over the past few decades, cancer cases from HPV have significantly increased as more people engage in unprotected sexual incidences. The World Health Organization indicated that around 12,000 males and 19,000 females in the United States suffer from the virus. Besides, other countries worldwide are also struggling with HPV (Araldi et al., 2018). The intensity of the virus and its effects, especially amongst the young populace, necessitates a discussion of vaccination’s cost-effectiveness against the virus. The evaluation banks on the US’s current statistics regarding the virus and its prevalence amongst people living in the US. It considers the present economic and health effects of the virus on the said populace to determine the viability of vaccination as the primary method of protecting the sexually active population against the virus.
Statistics of the US show that vaccination is a viable option for protecting women and girls against human papillomavirus. The age-group that deserves the most attention ranges between 9-26 years. The criteria for deciding the minimum age is that girls at the age of 9 are barely exposed to sex (Chesson, 2008). The efficacy of the vaccine is, for this reason, at its highest level. Similarly, most women are exposed to sexual activities before getting to 26 years of age. The available vaccines demand that the beneficiaries should embark on a series of immunization activities (Dasbach, Elbasha, & Insinga 2006). The years between allow time for the young women to complete the full vaccine series. The age range includes sexually active people. They are vulnerable to various sexually transmitted illnesses and likely to fall victim to the virus and its related infections. Taking into consideration the said age group maximizes the effectiveness of vaccination by ensuring that only the right persons receive the vaccine.
Statistics indicate that about 24.9 million girls and women are infected with human papillomavirus. The prevalence of infection is in the people who are aged between 20 and 24 years. The prevalence of the high risk of contracting the virus increases with an increase in age, up to 26 years of age (Chesson, 2008). However, after 26 years, the prevalence reduces, owing to factors such as the reduction in promiscuity and maintaining one partner. Within the number of infected women, about 25,400 of them have been diagnosed with cervical cancer. Cervical cancer is the most prevalent aftermath of getting infected with human papillomavirus (Lehtinen et al., 2018). It means that the vaccination processes should be directed towards reducing cervical cancer as opposed to any other type of cancer.
The costs associated with vaccination includes several cumulative costs. Among them is the cost of researching the most effective vaccine. Research conducted by Wigle, Coast, and Watson-Jones (2013) indicated that Certavix is the best vaccine. The research indicated that the bivalent HPV vaccine could effectively prevent against type 16 and 18 varieties of HPV. Being the most dangerous strains, it means that the vaccine can effectively prevent a large number of women and girls against the virus and its related fatal illnesses. The vaccine is also proven to be effective in preventing genotypes 6 and 11. Proof of its effectiveness is in the observed licensure and adoption in over 120 countries around the world. Among them, 51 countries have adopted the vaccine into their national HPV vaccination programs (Rambout et al., 2007). 26 countries are already implementing pilot programs in an effort to test the possibility of universal delivery strategies and potential ways of overcoming the potential challenges of effective delivery. The presence of well-researched information regarding the vaccine is a good basis for considering its use in the US.
The massive use of the vaccine in the US faces an assortment of challenges. Among the barriers to effective implementation of the plan to vaccinate girls and women are the existent sociocultural barriers (Giambi et al., 2014). US society demands massive sensitization regarding the vaccine. The population is characterized by inadequacy of information amongst parents and rumors regarding the negative effects of vaccination. It means that there is an urgent need to come up with strategies on how to effectively educate the population on the benefits of the HPV vaccine. The education can best be implemented through the education of people at all levels, beginning with the young girls to their parents. Barriers within the health system may also minimize the effectiveness of the application of vaccination as the best method of preventing HPV. Among them are the inadequacy of infrastructure and human resources and difficulties in financing systems. Political will may also minimize the effectiveness of the immunization programs if the politicians do not favor its implementation. However, the barriers are subject to removal and subsequent implementation of a well-developed vaccination program.
Ethical Perspective Inquiry
The epidemiological Perspective of vaccination of women and girls against human papillomavirus encompasses both the practice’s positive and negative aspects. On the bright side, the universal vaccination of the two vulnerable groups is done in good faith. For this reason, it is an acceptable activity from the ethical Perspective (Navarro-Illana, Aznar, & Díez-Domingo, 2014). It assists in the protection of women and girls against the illnesses that result from the virus. It is mostly preferred for its effectiveness in the process of protection. It is the best fit for the sexually active persons in their quest to maintain their productivity in child-bearing activities. HPV is common amongst the group of persons who are in their productive ages. Although effective, condoms offer a less viable solution in preventing the virus since productive copulation is necessary for propagating families. It offers the alternative of vaccination to help the persons remain productive while still preventing them from the dangerous virus.
The negative aspect of vaccination programs is that it has a deterrent effect. Eliminating the fear of developing cancer amongst teenagers may encourage underage sex (Salwa & Al-Munim, 2018). The question that arises from this worry is whether it is ethical to remove the deterrent effect that would have minimized sexual activities amongst young people, especially adolescents. In one aspect, it is arguable that vaccination has more advantages than disadvantages. It minimizes fear from amongst the people and replaces it with confidence about the future. It also minimizes the risk of developing a fatal illness. Taking away the fear is, for these reasons, a good activity. On the contrary, it is also arguable that fear is a useful medical measure, owing to its ability to discourage underage sex and multiple sexual partners. The usefulness of fear in medicine improves the welfare of young people. Removing it from amongst them can result in promiscuity, which has worse effects on the young persons. For this reason, it is not ethically acceptable to promote the universal vaccination of women and girls against the human papillomavirus.
A related aspect of the ethicality of vaccination is that sex is a spiritual issue that should be evaluated from an ethical perspective. Sex has both physical and spiritual; importance. The physical aspect is all about pleasure. From the spiritual Perspective, sex satisfies the need for human beings to express love. The vaccination of women and girls against human papillomavirus has a double effect on human beings’ sexual activities (Salwa & Al-Munim, 2018). It can encourage the engagement of sex amongst the underage populace. For this reason, it is not merited in the moral aspect since it has a negative side effect. In the least, it should not affect the welfare of people in their sexual engagements. This negative effect is further discouraged based on the presence of other alternatives to achieve the same product. The targeted groups of women and girls can be educated on other alternatives to preventing the fatal illness. The alternatives, such as condoms and avoiding promiscuity, have positive effects that are morally valid.
Another perspective of the issue of vaccination is the possibility of informed consent. A significant percentage of the available vaccination programs barely offer significant information and autonomy to the recipients. Instead, they tend to be enforced on people, especially in areas where the populace is not well financially endowed (Navarro-Illana, Aznar, & Díez-Domingo, 2014). The case of universal vaccination of women and girls in Bangladesh exemplifies this ethical issue. Some organizations do not put adequate measures to ensure the satisfaction of the need for proper information before the administration of the vaccines. However, the people implementing the programs can be excused from the blame based on the difficulty of obtaining consent from the targeted populace. In most cases, it is difficult to obtain consent from adolescents and their parents and guardians before administering HPV vaccines. The issue has an ethical perspective since it involves making a decision or being coerced to receive the vaccine.
An extension of the argument is that parents have an inalienable right to decide whether their children will receive the vaccination. Parents have dominion on issues related to sex. They have an inalienable right to decide whether their children should get sex education and whether they should receive the HPV vaccine. In most cases, vaccination programs barely incorporate this aspect of consent. In Bangladesh, for example, the vaccination programs use implied consent (Salwa & Al-Munim, 2018). It means that parents are told about imminent immunization through public communication. There is no written procedure for ensuring that the parents are in tandem with the authorities involved in their daughters’ immunization. It means that the programs tend to take away the parents’ rights to decide for their daughters, which is morally wrong. It is especially worse if the daughters receive sexual education, intending to create awareness amongst them. Failure of the programs to consider the parents’ rights over their children is the ethical issue that demands to be addressed.
Conclusion
Human papillomavirus is a major health challenge amongst most sexually active persons in the US. The virus is a stealth killer that is transmitted through contact. Most of the infected persons are unaware of the infection. It is from this lack of awareness that the persons transmit the virus. The result is the widespread prevalence of various fatal illnesses. The most significant of them is cervical cancer. However, efforts towards prevention against the illness are being put in place. The most promising of them are researching, developing, and administering vaccines. Vaccination programs promise the provision of a superior method of prevention against human papillomavirus by allowing sexually active persons to engage in sexual practices without the fear of developing cervical cancer. However, implementation of HPV vaccination programs is subject to criticism, owing to the question of the practice’s ethicality. Some fear that the practice may encourage early sex and promiscuity and take away the right of parents and adolescents to decide for themselves on sexual lessons and vaccination.
Various authors have different conclusions on the viability of vaccination programs as the primary method of preventing human papillomavirus spread. However, the universal agreement is that the program is viable in the US. Its implementation is cost-effective and applicable both in the short and long-term. Going by the calculations, it is agreeable that a vaccination program is viable in the US. Already, reputable researches are explaining the best vaccine that will be most effective if applied. Using such researches promises a good future for the US population. According to Wigle, Coast, and Watson Jones, the program’s implementation is challenging, owing to the barriers that face it. However, this conclusion may be faulted for failure to incorporate the environment of the US in full. The barriers are strongly inclined towards other less developed countries that are marred by political upheavals. The authors offer good ways of interpreting the results. However, the results might have been more comprehensive if the interpretations included information on the vaccination program’s long-term effects. The likelihood of affecting the country’s budget is a major factor that demands careful consideration.
The researches used in this study include some significant weaknesses. Among them is the failure to include an in-depth evaluation of the significant challenges that may affect the implementation of the vaccination programs in the US. Only one research identifies potential challenges. It is also weak in that it does not narrow down the information to the situation in the US. Another weakness is the failure to address the possibility of eliminating the weaknesses of the program. It would have been better if the researchers explained the possibility of changing the situation to benefit vulnerable girls and women. They propose the creation and implementation of a cost-effective vaccination program. I agree with them on that. However, I believe that there is a better chance of addressing the issue of vaccination by forging how the concerned parties can collaborate for the better effectiveness of the program. It means that scientists will research and develop the vaccines, and other people will engage the public in awareness creation, while others will take care of the ethical aspect of the HPV vaccines. Doing so will ensure a holistic approach to the contentious issue.