Research Critiques and PICOT Statement
Introduction
The purpose of this paper is to combine the synthesis of four articles that examine the issue of nurse burnout and the strategies to manage and prevent burnout. Addressing burnout is significant because it will benefit the nurses and other healthcare professionals in identifying the risk factors and learning about various strategies for coping with burnout and preventing burnout. Consequently, nurses will become more satisfied with their jobs and have a positive mindset about their profession, which will increase the quality of patient care.
Nursing Practice Problem and PICOT Question
Burnout, which is a common phenomenon within the healthcare profession, is described as a chronic-work related stress that causes healthcare providers to feel emotionally exhausted, depersonalized, and lose interest after thy have been exposed to stress for a long time. Healthcare providers have been particularly prone to burnout as a result of excessive and overwhelming demands that are necessary in this profession. Among healthcare providers that are a high risk for burnout are nurses. Nurses work in highly stressful environments that demand their physical, emotional, mental, and spiritual strength in making decisions that impact the lives of their patients. As a result of these stressors, the nursing practitioners are at a high risk for burnout. Nurse burnout is a serious issue that nurses, employers, and patients are all concerned about. Nurses are at risk of developing depression and other mental health problems, losing passion for their jobs, and quitting their jobs. For healthcare organization, nurse turnover as a result of burnouts causes a decrease in patient care quality, poor reputation, and a decreased profitability. For patients, nurse burnout can directly affect the quality of care they receive. Since nurse burnout is becoming more prevalent, there is a greater need for intervention to reduce nursing burnout levels.
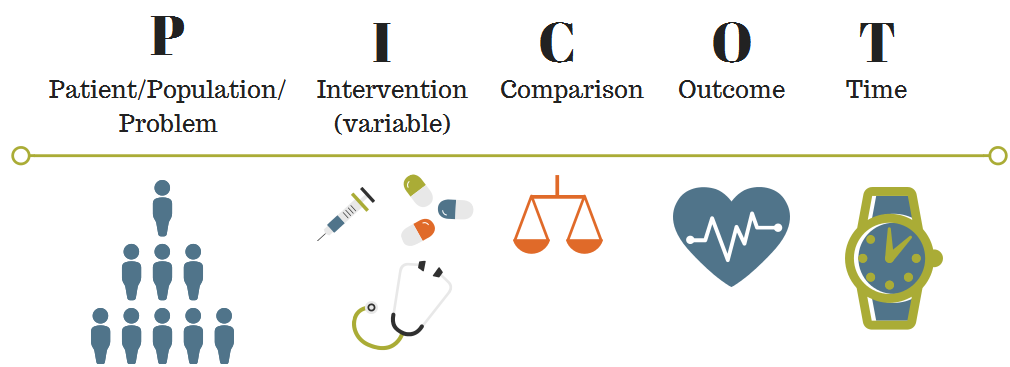
PICOT Question
Are coping mechanisms effective in reducing nursing burnout among nurses who practice burnout coping mechanisms compared to nurses who do not practice burnout coping mechanisms over a period of six months?
P: Nurses
I: Burnout coping mechanisms
C: No burnout coping mechanisms
O: Reducing nursing burnout
T: Six months.
Background
Burnout and compassion fatigue have a substantial effect on healthcare professionals, their families, and patient care quality, particularly in the critical care settings such as Intensive Care Units (ICUs) (Hancock, et al., 2020). This study is significant to the nursing profession, as the design of successful interventions for team resilience among nurses can be guided by understanding burnout and compassion fatigue. The objective of this study as stated in its purpose statement was to investigate at the organizational and personal factors that lead to burnout and compassion fatigue among a Canadian academic intensive care unit (ICU) healthcare staff. The researchers were guided by the following question: What are the individual and organizational level factors that contribute to burnout and compassion fatigue in the ICU healthcare team? (Hancock, et al., 2020).
Burnout is common in critical care settings and the impact of resilience as a possible solution to burnout (Jackson, et al., 2018). The study’s significance is based on the fact that burnout and resilience are predictors of the management of adversity in the healthcare environment. Adversity has a negative influence on healthcare providers and should be dealt through interventions in the healthcare environment. Burnout and resilience are evidence of a constructive strategy to resiliency and burnout prevention. The objective of this study as stated in its purpose statement was to understand more about nurse burnout and resilience in response to adversity in acute care settings. The researchers were guided by the following question: What is the effectiveness of resiliency in preventing workplace adversity among nurses in the acute care settings? (Jackson, et al., 2018).
Incivility has adverse implications in the nursing work environment workplace, and it is still a problem in the nursing profession. Incivility has long been connected to nurse burnout, which leads to poor mental health and nurses’ intention to voluntarily change their profession or organization. It is vital to understand what elements can safeguard nurses from the adverse effects of incivility to promote retention of talented and highly competent nursing professionals (Fida, Laschinger, and Leiter, 2018). The study is significant because nurses’ levels of occupational coping self-efficacy may have a substantial impact on their understanding and coping with occupational stress arising from their interpersonal connections, and therefore also on their outcomes. The purpose of this article is to examine the function of interpersonal workplace coping self-efficacy in protecting nurses against incivility, burnout, and turnover intentions. Its objective is to focus more on the potential protective impact of interpersonal workplace coping self-efficacy in a stressful nursing work environment. The study was guided by the following research question: What role does interpersonal workplace coping self-efficacy play in preventing workplace incivility, burnout, and turnover intentions? (Fida, Laschinger, and Leiter, 2018).
Stress has become an inevitable component of working as a nurse. Workplace stress that is experienced on a regular basis might cause burnout (Geuens, et al., 2020). While environmental stressors have a significant impact on burnout, their capacity to predict burnout is very restricted. This study is significant since it hypothesized that core self-assessments, coping strategy, and situational factors are all important indications of burnout. Its purpose is to investigate how individual susceptibility variables, such as core-self assessments and coping, relate to burnout in hospital-based nurses in response to contextual stressors. Its objective is to explain the the connection between core-self assessment, coping strategies, situational factors, and burnout within the nursing field. The study was guided by the following research question: What is the impact of core-self assessments factors and coping on nursing burnouts? (Geuens, et al., 2020).
Article support of the Nurse Practice Issue
There are different effective strategies for coping with burnout and compassion fatigue in an acute care setting. The PICOT question can be informed through information about the self-constructive strategies that can be implemented for nurses in critical care settings as well as other settings to improve coping with burnouts and employee retention (Hancock, et al. 2020). Some coping strategies to nursing burnout result from adversity in the acute care settings. The PICO question can be informed by providing information about the coping strategies that can be used by nurse leaders to build resilience or to avoid emotional exhaustion, disengagement, and low self-actualization, among nurses, based on their strengths and qualities (Jackson, et al., 2018). The PICOT question can also be answered by examining the function of interpersonal workplace coping self-efficacy in protecting nurses against incivility, burnout, and turnover intentions. In this way, evidence on how interpersonal workplace coping self-efficacy is effective in helping nursing to cope with incivility, burnout, and turnover intentions is important (Fida, Laschinger, and Leiter, 2018). Finally, the PICOT question can be answered by investigating how individual susceptibility variables, such as core-self assessments and coping, relate to burnout in hospital-based nurses in response to contextual stressors. In this way, evidence on the impact of elements of vulnerability such as coping in addressing burnout for hospital-based nurses can answer the PICOT question (Geuens, et al., 2020).
According to the PICOT question, the intervention group consists of nurses who practice burnout coping mechanisms while the control group consists of nurses who do not practice burnout coping mechanisms. The participants in the study by Hancock, et al (2020) were physicians, ICU nurses, and respiratory therapists while participants in Jackson, et al. (2018) were female acute care nurses as participants. Since these studies were qualitative, the experiences and perceptions of the participants were investigated and interviews with others who lacked experience were considered uninformative (Busetto, Wick, & Gumbinger, 2020). Therefore, it was not relevant to have control groups in both studies. In Fida, Laschinger, and Leiter (2018) and Geuens, et al. (2020) studies, there were no intervention and control groups because the studies were not designed as randomized control trials to test interventions between the experimental group and a comprisson group. Instead, participants were Canadian nurses who were asked multiple survey questions and nurses from 11 Belgian hospitals selected to paricipate in a population-based survey in Fida, Laschinger, and Leiter (2018) and Geuens, et al. (2020) respectively.
Method of Study
Hancock, et al. (2020) conducted a qualitative study using focus groups to gain participant opinions on burnout and compassion fatigue in the ICU teamwork context. The researchers conducted thematic analysis of transcripts obtained from their focus groups with physicians, ICU nurses, and respiratory therapists, which accounted for the causes of burnout and compassion fatigue, their impact, strategies to cope, and the recommendations for building high resilience (Hancock, et al., 2020). Jackson, et al. (2018), utilized the grounded theory research through the Corbin and Strauss methodology. Qualitative, open-ended interviews were conducted with the participants to gain insights about nursing burnouts and resilience (Jackson, et al., 2018). Fida, Laschinger, and Leiter’s (2018) study is a longitudinal study, in which nurses completed two mail surveys, one at the baseline, and the second after two years. The researchers used multivariate statistical analysis for testing the hypothesized model. Geuens, et al’s. (2020) study is a cross-sectional study using five self-report measures: Dutch Core Self Evaluations Scale, Nursing Work Index Revised, Utrecht Coping List, Ruminative Response Scale, and Utrecht Burnout Scale.
Focus groups provide methods to gather data from group interactions that are focused on the researcher’s topic of interest. However, it is impossible to tell whether the members in the interaction group are thinking about their own conduct. The contextual nature of knowledge, and also the contingent nature of conduct, can be identified using grounded theory. However, grounded theory methods generate a lot of data, which can be challenging to handle (Busetto, Wick, & Gumbinger, 2020). Longitudinal studies are beneficial in that they enable researchers to track and monitor their subjects in actual time when the study occurs. This implies that it is easier for the researcher to establish the actual sequence of events, and measure the relationship between two phenomena. However, since longitudinal studies take longer and are generally more expensive than other study designs, they necessitate a large amount of time and funding to be successful. Cross-sectional surveys, on the other hand, do not track participants over time and are normally inexpensive and simple to perform. However, biases such as responder bias, recollection bias, interviewer bias, and social acceptability bias can affect them (Tarris, Kessler, & Kelloway, 2021).
Results of Study
The study by Hancock, et al. (2020) found out that working in a burnout-prone and low-morale environment has a negative impact on healthcare personnel’ physical and mental health, as well as their relations with friends and families and patient care. The self-constructive strategies for coping with burnouts are adequate staffing, providing education and training for the healthcare professionals, promoting teamwork, and meaningful recognition. The study by Jackson, et al. (2018) found out that for acute care nurses, resilience and burnout are linked as indications of the same process. Nurse leaders can act at any point in the process to help nurses cope with stress in their profession and build resilience. The key findings of the study by Fida, Laschinger, and Leiter (2018) are that interpersonal workplace coping self-efficacy is a critical protective factor against incivility, burnout, and turnover intentions. Geuens, et al. (2020) found out that burnout is predicted by core self-assessments, situational circumstances, and coping. Emotional exhaustion is strongly linked to core-self assessment. Core-self assessments could be used at the start of the loss cycle.
Concerning the implications of the studies, according to the study by Hancock, et al. (2020), the implementation and evaluation of the impact of the self-constructive strategies for coping with burnouts, including adequate staffing, providing education and training for the healthcare professionals, promoting teamwork, and meaningful recognition is the basis of preventing future burnout and compassion fatigue. The study by Jackson, et al. (2018) has some clinical implications for nurses. Burnout and resilience are predictors of adversity-management process, although they may not automatically indicate a nurse’s coping abilities. Adversity in the healthcare environment is detrimental to acute care nurses and should be addressed through interventions in the healthcare environment. Burnout and resilience are evidence of a constructive strategy to resiliency and burnout prevention. Fida, Laschinger, and Leiter’s (2018) study can be used to increase self-awareness of how to cope with occupational stress. Hospital managements should make substantial efforts to establish work environments that discourage or prevent incivility, burnout, and turnover intentions. Geuens, et al.’s (2020) study will serve as the foundation for planning and implementation of requisite measures by hospital managements to better adapt healthcare professionals to the nursing field and enhance their health, both of which are requisite to providing high-quality nursing care. The loss and gain cycles should be used as a framework for both personal and organization-oriented interventions to obtain insight into the how burnout develops.
Ethical Considerations
Researchers are sometimes uninformed about breaking ethical research guidelines. The moral standards that guide researchers in conducting and reporting research without dishonesty are known as research ethics. It is critical to follow ethical principles when conducting research in order to ensure the validity of a study (Yip, Han, & Sng, 2016). Informed consent and confidentiality are two of the most common ethical considerations that must be taken into account when a study includes human participants. The imperative to get informed consent stems from a respect for individuals and willingness to safeguard the autonomy of individuals who choose to volunteer for research (Kadam, 2017). Accordingly , no one may be forced to participate in research against their will. Confidentiality refers to an agreement between the researcher and the participant that ensures sensitive and personal information is used and managed with extreme caution (Burles & Bally, 2018). Any information about a person’s personal life that they do not want exposed to others is deemed “confidential.”
In Hancock, et al. (2020), the researchers first sought approval from the Research Ethics Board. Subsequently, before the beginning of the focus group discussions, written informed consent was sought. In the study by Jackson, et al. (2018), the researchers initially sought approval from the Athabasca University research ethics committee, as well as the hospital research ethics committee. The researchers then provided the participants with information sheets and invitation notes for participating in the study. The sheet was reviewed during a meeting between the researcher and the participants. Then, participants provided written consent to take part in the study. They were assured that their information would be kept confidential and no personal or sensitive information would be revealed to others or included in publications. Fida, Laschinger, and Leiter (2018) sought approval from the university ethics board and later provided participants with information about their study and the need for voluntary participation. Geuens, et. (2020) collaborated with the nursing unit managers, and announced their survey to the participating nurses. They were required to sign informed consent forms and informed that they should only participate in the study at their own will.
Outcomes Comparison
According to the PICOT Question, the anticipated outcome is reducing nursing burnout. Burnout is a complex issue, and is one of the leading causes of poor performance among healthcare professionals. Addressing the burnout syndrome requires multiple interventions (Bakhamis, et al., 2019). Effective interventions can help to reduce nurse burnout and improve the quality of care offered in health facilities (Kim, et al., 2020). Reduced burnout is associated with lower turnover rates, higher patient Satisfaction, safe and quality care, and improved mental health over a long period of time.
The outcomes of the four articles support the significance of reducing burnout among nurses. The self-constructive strategies for coping with burnouts are adequate staffing, providing education and training for the healthcare professionals, promoting teamwork, and meaningful recognition (Hancock, et al., 2020). Nurse leaders can act at any point in the process to help nurses cope with stress in their profession and build resilience (Jackson, et al., 2018). Interpersonal workplace coping self-efficacy protects against incivility and turnover intentions, and reduces burnout (Fida, Laschinger, and Leiter, 2018). Core-self assessment, coping, and situational factors are significant in predicting and reducing nursing burnout (Geuens, et al., 2020).
Proposed Evidence-Based Practice Change
The PICOT question, the research articles, and nursing burnout are connected. Burnout and compassion fatigue have a substantial effect on healthcare professionals, their families, and patient care quality, particularly in the critical care settings such as Intensive Care Units (ICUs) (Hancock, et al., 2020). Burnout is common in critical care settings and the impact of resilience as a possible solution to burnout (Jackson, et al., 2018). Incivility has adverse implications in the nursing work environment workplace, and it is still a problem in the nursing profession. Incivility has long been connected to nurse burnout, which leads to poor mental health and nurses’ intention to voluntarily change their profession or organization (Fida, Laschinger, and Leiter, 2018). Stress has become an inevitable component of working as a nurse. Workplace stress that is experienced on a regular basis might cause burnout (Geuens, et al., 2020).
It is therefore vital to understand what elements can safeguard nurses from the adverse burnouts and its related impacts. Accordingly, the recommeded evidence-based practice change is improving the identification of the risk factors for burnout and improving interpersonal adequate staffing, providing education and training for the healthcare professionals, promoting teamwork, effective leadership, resilience building, meaningful recognition, and workplace coping self-efficacy.
Conclusion
Burnout is predicted by core self-assessments, situational circumstances, and coping. Emotional exhaustion is strongly linked to core-self assessment. Addressing burnout is significant because it will benefit the nurses and other healthcare professionals in identifying the risk factors and learning about various strategies for coping with burnout and preventing burnout. Nurse burnout can be managed and prevent burnout through interpersonal adequate staffing, providing education and training for the healthcare professionals, promoting teamwork, effective leadership, resilience building, meaningful recognition, and workplace coping self-efficacy, which is a critical protective factor against incivility, burnout, and turnover intentions.






