Quality and Sustainability in Nursing Science and Healthcare System – Analysis and Application
Introduction
Currently, the primary focus of the healthcare system is to address the rising costs of healthcare while enhancing desirable patient outcomes. This has consequently led to the rapid development of quality measures. There is an increased interest in quality measurement, which has been, which has been influenced by the rising ability to measure and analyze healthcare quality. Additionally, advances in health technology have facilitated the increased use of technology in healthcare (Quentin et al., 2019). Quality measurement differs in different organizations, since different healthcare facilities have different functions. Information from quality measurement is used for accountability and to assess the quality of care being delivered by an organization. Quality and safety play a significant role in nursing science.
Part One – Quality and Safety: Fall Prevention
Defining Quality and Safety Measures and their Relationship to Nursing Science
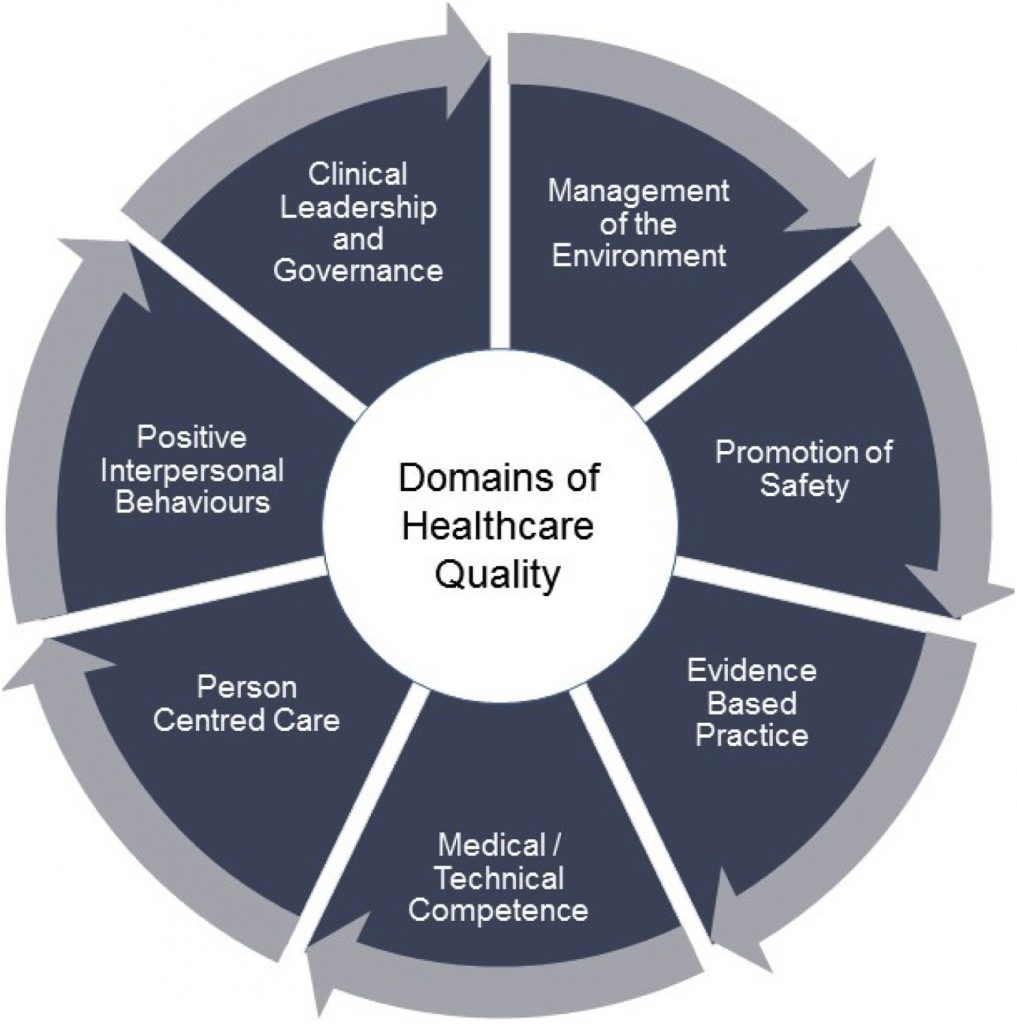
Quality measures can be defined as the tools that are used to measure or quantify healthcare processes, outcomes, patient perceptions, and organizational systems that are associated with the provision of high-quality healthcare. Quality measures are categorized into three types; structure, process, and outcomes. All three measures are vital in assessing the quality of patient care (Adirim et al., 2016).
Structural measures assess the adequacy of organizational resources in improving patient outcomes. This includes assessing the type of care that an organization provides, as well as specific systems such as electronic health records, which improve care. Process measures assess how the practitioner and the patient interact. Additionally, process measures assess the practitioners’ use of standard protocols when assessing patients, how healthcare services are provided, as well as the ability of a patient to access healthcare services. Outcomes measures assess the effectiveness of the delivered healthcare services, and these may either be immediate or long-term outcomes (Adirim et al., 2016). Through quality measures, healthcare facilities are able to benchmark their performance against other facilities. Additionally, quality measures are used by consumers and insurers to evaluate the performance of healthcare facilities.
Nursing care is vital in ensuring that patients achieve quality outcomes. Therefore, measurement of the quality of care delivered results in the assurance of performance in nursing care. The American Nurses Association (ANA) Social Policy Statement asserts that nurses have a responsibility to advance the art and science of nursing, and in exchange, the public expects to receive quality care (Jones, 2016). When measuring performance, the outcomes measured are inherent to the definition of nursing. Nurses have an obligation to measure interventions in health promotion, illness and injury prevention, and alleviation of suffering. When performance measurement results in the improvement of quality of care, then measuring nursing outcomes is considered beneficial. Performance measurement using quality measures makes problems within an organization visible to stakeholders. This consequently drives selective attention to nursing care which leads to selective improvement.
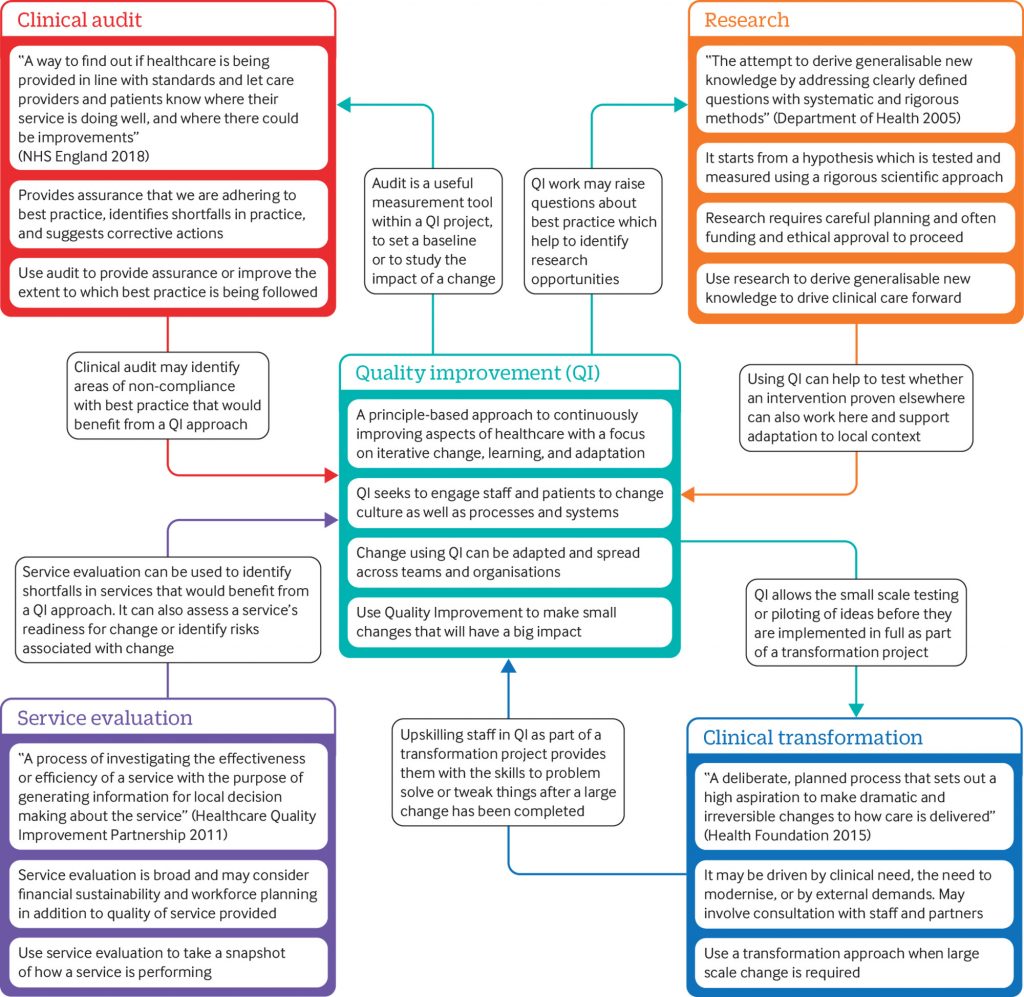
While quality measures are vital in improving healthcare services’ delivery, nursing care is more challenging to measure and conceptualize. This is because most nursing interventions are not technical, but instead, they involve information transfer, which can be challenging to measure. For quality measures to function efficiently, they should have a clear definition, and in addition, they should provide credible and consistent estimates of performance. Useful measures provide information that is actionable. Jones (2016) explains that for a long time, nurse leaders have understood the importance of measuring nursing care outcomes. Nurses have a social responsibility to assess how nursing practice affects patient outcomes. While in most healthcare facilities, nurses lack direct control over the total outcome of care, individual actions can improve outcomes. Nurses can also improve process measures by the development of quality improvement initiatives with interprofessional team members, which can result in improved patient outcomes. More importantly, the use of quality measures can improve the implementation of evidence-based practice since process measures can provide evidence that can drive nurses to continue implementing best practices.
Application of Quality and Safety Measures in Nursing Science
Quality and safety measures are utilized to monitor and improve the quality of healthcare services. The most commonly used domains of improving healthcare are safety, the process of care, outcomes, and patient experience. When selecting measures, it is crucial to ensure that they reflect the goals of the practice institution. Critical nursing practice can be measured by assessment of fall prevention. Nurses play a significant role in ensuring patient safety. Prevention of falls and fall-related injuries is an important nursing role. Patient falls are a significant health problem; hence nurses contribute to patient safety by assessing patients’ fall risk and designing patient-specific interventions to reduce the risk of falls (Quigley & White, 2013). Fall-related data within health care facilities is collected through incident reports. Data collected through incident reports is evidence-based and includes factors that contribute to fall occurrences.
Quality measures in nursing practice can, therefore, be applied by counting and tracking fall rates and fall prevention practices. Measuring fall-related injury rates is a direct measure of how healthcare providers are ensuring patient safety with regard to falls. Improving rates indicate that falls and fall-related injuries are prevented accordingly. Within a healthcare facility, falls should be measured so that they can be compared over time. For instance, nursing staff can track the number of falls every month. Some of the structural measures for establishing fall rates include nurse to patient ratio, fall present on admission, and interprofessional members on a fall team. Additionally, some of the process measures associated with patient falls include fall risk assessment/ reassessment, fall injury risk/history assessment, and fall injury prevention interventions. Outcomes measures include fall rate per 1000 patient days, modifiable risk factors reduction, and the number of days between major fall injuries (Quigley & White, 2013).
Quality Components Needed to Analyze a Healthcare Program’s Outcomes
Analyzing the outcomes of a healthcare program helps identify the effects of the program. Outcome measures help determine whether there are changes in the health of an individual, or a group of people, which are attributable to a specific intervention (Adirim et al., 2016). The components required for analyzing the outcomes of a healthcare program include the problem, the goal, the aim, the measurements, and the analytics. The problem provides a foundation for the entire healthcare program and ensures that the right program is implemented. If the problem is analyzed appropriately, the outcomes of the program will result in the resolution of the problem. Failure to address the problem accordingly will result in outcomes that are unrelated to quality patient care. Goals guide the program implementation process; hence the program outcomes should indicate achievement of the goals. The aim helps assess whether the program implementation process utilizes less time and costs. The measures, on the other hand, provide information on whether the outcomes indicate improvements. Finally, analytics helps analyze the overall care quality, patient experience, and the effectiveness of the improvements.
Part Two – Analysis and Application
This part of the paper analyzes the quality outcomes of First Care Medical Center (FCMC), a healthcare facility that offers comprehensive health care services to patients residing in Santa Clara. Other aspects analyzed include the facility’s successes and failures, potential obstacles to the implementation of quality and safety measures, and the collaborative efforts needed to create sustainability within the facility.
Description of the Healthcare Entity
FCMC is a healthcare entity located in Santa Clara, Florida. The facility is an acute care medical center that offers compassionate care to people residing in Santa Clara Valley. FCMC is a 121-bed facility offering emergency medicine, trauma care ad acute care surgery, urgent care, prehospital care, and critical care. It is the most preferred healthcare provider in the region. The facility plays a significant role in the prevention of death and disability among residents living within its locality. FCMC has been in operation for sixteen years, and throughout this period, it has benefited a large number of Santa Clara Valley residents. The organization is for-profit; hence the main goal of the facility is to make profits while delivering quality services to community members. This allows the facility to operate efficiently and manage the revenue cycle.
FCMC’s Successes and Failures
The facility prides itself in the delivery of the most comprehensive healthcare services within the region. The healthcare system at FCMC is designed to foster teamwork and collaboration, such that the patients’ needs are adequately addressed from a holistic perspective. Patient-reported outcome measures (PROMs) indicate that patients are highly satisfied with the care provided by healthcare professionals at FCMC. An assessment conducted within the facility six months ago shows that care provided within the facility meets individual needs and expectations. Patients who visit the facility receive a higher level of commitment and care from the providers. The primary goal of healthcare providers within the facility is to ensure patient satisfaction. Patient satisfaction is linked to key success metrics for healthcare providers.
The facility has been unable to adopt technology use, which has significantly affected its ability to ensure that the services delivered are optimal. Additionally, increased readmission rates is a major failure that the organization has been striving to address success has been minimal. Over the last five years, the hospital has recorded an increase in the 30-day all-cause readmission rate by 12.5%. Currently, high readmission rates at FCMC is a major burden that is associated with poor patient outcomes and increased costs. According to Fischer et al. (2014), the risk of getting readmitted varies between patient groups and conditions. Data within the facility also indicate that the risk for readmission is high for patients with low socioeconomic status, advanced age and comorbidities. The inability of the organization to integrate programs that can address the issue of high readmission rates has affected its overall credibility.
Quality/Safety Area that Nursing Science can Impact
As mentioned earlier, an area of concern within the facility is increased rates of readmission within 30 days of discharge. Reducing readmission rates should be a priority for the facility, as this is an essential quality indicator. This can be achieved through the implementation of various care coordination programs, such as the discharge companion program, which utilizes a transitional management model. This model emphasizes on interprofessional collaboration. Nurses play a significant role in the discharge planning process. The transitional management model addresses various barrier in a client-centered manner. Such barriers include transportation issues, polypharmacy, finances, health beliefs, emotional and spiritual health and self-concept (Stixrood, 2019). The mentioned tremendous increase in readmission rates indicates that the facility needs to focus on practice guidelines that can reduce patient readmissions within 30 days of discharge. It is critical for nurses to implement strategies that allow patients to understand the whole process since better awareness creates a smooth transition.
Potential Obstacles
While readmission rates can be avoided, some of the barriers to reducing readmission rates include scarce resources, a variety of patient needs, the facility’s limited ability to influence care in the community, and misalignment of financial incentives. The limitation of personal and financial resources will be a significant challenge that will impact the implementation of an initiative to reduce early readmissions. For instance, the initiative may require the collaboration of social workers, nurses, other outpatient staff, and project managers, who will require financial compensation. Different patients have varying care needs. The fact that healthcare professionals have a limited ability to control patient characteristics such as homelessness, lifestyle modification, medication nonadherence, and substance abuse will make it difficult for them to address the issue of readmissions. Additionally, considering each patient’s unique needs, it can be challenging to determine the interventions that will be effective for each patient (Joynt et al., 2014).
It is worth noting that factors outside the facility are difficult to change. These include aspects such as the lack of access to primary care will inhibit the successful implementation of a readmissions rate reduction initiative. The lack of a primary care provider for most of the patients visiting the facility increases their likelihood of being readmitted after discharge. According to Joynt et al. (2014), one of the most essential factors in reducing hospital readmission is access to outpatient care. Another challenge that may affect the success of initiatives in reducing readmission rates is the misalignment of financial incentives. For instance, the facility’s environment is fee-for-service, which sorely depends on the number of admissions. Therefore, facility administrators may argue that the reduction of readmissions will result in the loss of revenue, which can consequently outweigh any penalties incurred. These negative financial implications for the facility may hinder the implementation of initiatives to reduce readmission rates.
Collaborative Efforts
When implementing an initiative to reduce readmission rates, it is crucial to collaborate with organizational leaders and other stakeholders to ensure more success. Programs such as transition of care (TOC) help in the reduction of readmission rates. While most care coordination programs offer patient support in medication adherence during the first few days after discharge, assistance beyond five days is vital in reducing readmission rates (Bingham et al., 2019). Medication management is especially a problem for most patients; hence including a pharmacist-in-charge in the readmission rates reduction plan is crucial. Such collaboration is vital in improving overall patient safety and reducing healthcare-related costs.
The role of the pharmacist, in this case, is to conduct the patients’ medical safety evaluation while addressing several key components. These include drug-disease interactions, drug-drug interactions, high-risk medication use among the elderly, adverse drug events, dose appropriateness, and therapeutic duplications. The pharmacist will also help in the identification of barriers to medication adherence and consequently provide education to patients using the teach-back educational process. The pharmacist will also be responsible for contacting the patients after three weeks to assess any patient-related issues associated with medication nonadherence. Such issues include cost, new adverse drug events, and vaccination status. The pharmacist also addresses general questions that the patient may have (Bingham et al., 2019).
According to McCants et al. (2019), case management services are effective in reducing hospital readmissions. Therefore, it is vital to collaborate with case managers during the implementation of initiatives to reduce readmission rates. The case manager will help identify the appropriate providers and facilities throughout the continuum of care, depending on the needs of the patient. The case manager, therefore, ensures that resources are available in a timely and effective manner. When implementing an initiative to reduce readmission rates, the case manager will be crucial in identifying at-risk populations, thereby reducing the risk of readmission by addressing issues during hospitalization. A safe transition of discharge requires efficient collaboration between the facility’s case manager and the client, as well as the primary care provider.
Conclusion
The current healthcare system focuses on the provision of quality care in a sustainable manner. Quality outcome indicators such as patients’ experience and readmission rates ensure that healthcare facilities strive to provide the best available care to patients. FCMC prides itself in the delivery of patient-centered care, but the increasing readmission rates within the facility affect its overall outcomes. Problems such as increased readmission rates can be addressed through the implementation of programs whose focus is to ensure comprehensive discharge planning and implementation. For instance, coordinated care can help reduce unnecessary readmissions, but this can be achieved through the recognition of the importance of collaboration among healthcare provides. To ensure effective care provision, facilities must strive to conduct assessments that help recognize care inefficiencies. The data collected should then be used to design quality improvement initiatives, depending on the nature of the identified care gaps.