Background: Children with Autism Spectrum Disorder (ASD) need intensive behavioral interventions that can last for longer durations and help them acquire new skills. Since interventions are expensive, clinician-dependent, and not accessible amid COVID-19 due to traditional therapy centers’ closure, there is a dire need for plausible alternatives. A viable option is a home-based ABA program available on a mobile application, integrated with training videos and instructions. The program can be revised and personalized using Artificial Intelligence technologies to overcome traditional intervention models’ limitations.
Aims: The pilot study amid COVID-19 evaluates the efficacy of a parent-mediated home-based ABA intervention program facilitated through a mobile application. We explore Artificial Intelligence technologies’ role in automating ABA interventions’ personalization in language, behaviors, academics, social and life-skills.
Methods and procedures: This is a two-part study.
Fig 2. Study design using the longitudinal therapy data for Phase II of the study.
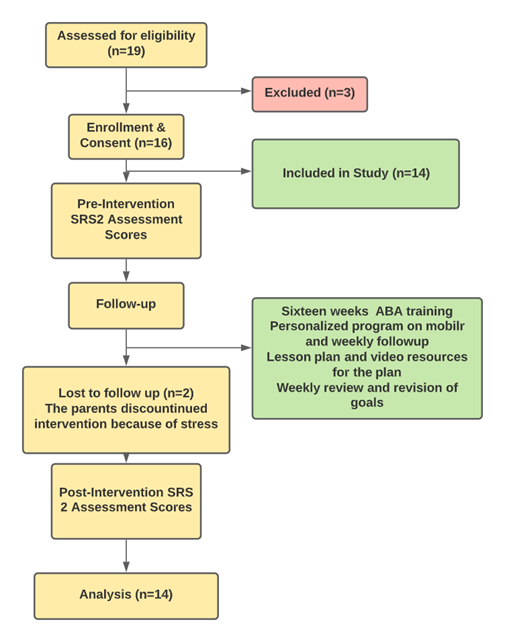
Part-1 We recruited fourteen children diagnosed with Autism who underwent parent-mediated ABA intervention amid COVID-19 facilitated through a mobile-application for sixteen weeks. Using the pre-post study design, we measured changes in Social Responsiveness Scale (SRS2) scores to assess the intervention’s efficacy.
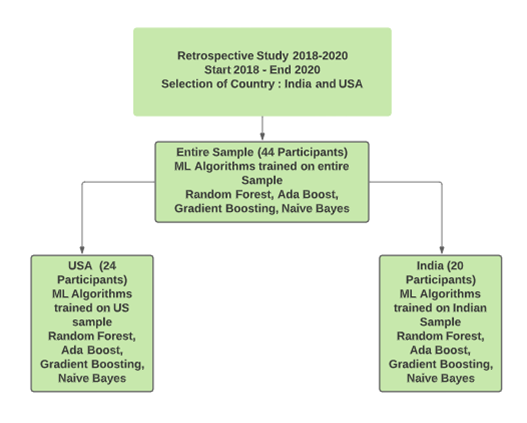
Part-2 As part of the longitudinal study design, we collected retrospective intervention data between 195 to 221 days of forty-four children, nineteen from India and twenty-five from the USA. We applied Machine learning models on the dataset to personalize the intervention plan and validated the outcomes using the cross-validation technique.
Outcomes and results: The outcomes of paired t-test (t=4.67, p=.00054), Cohen’s D (0.39), and Wilcoxon signed-rank test (p=0.001) demonstrate the efficacy of parent-mediated mobile-based ABA intervention. We also recorded ABA intervention personalization recommendations from machine learning models for 44 children from India and the US with 79.2% accuracy.
Conclusions and implications: A mobile-based parent-mediated ABA program integrated with personalized goals, pedagogy, and training resources can reduce Autism severity and enhance children’s skill acquisition. However, during the intervention period, a clinician must revise and personalize the ABA program regularly as per the child’s need. Machine learning models trained on the children’s longitudinal intervention data can generate recommendation models for clinicians to revise and personalize ABA programs and promote ABA interventions’ access and affordability.
Keywords:
ASD; Autism Spectrum Disorder; Applied Behavior Analysis; Machine-learning; Artificial Intelligence.
What contribution does this research make?
• Adds to the rehabilitation literature on the application and benefits of parent-mediated mobile-based ABA intervention to manage children diagnosed with Autism Spectrum Disorder (ASD) in the COVID-19 pandemic.
• Adds a new dimension to intervention literature on integrating machine learning technologies with longitudinal intervention data to develop self-learning recommendation systems to enhance the clinician capacity with the timely revision and personalization of ABA programs. The technological framework can reduce the dependence on limited clinicians, improve ABA intervention’s access, quality, and affordability.
Ethical considerations:
We have followed all necessary ethical considerations for this study. Before enrollment, the study staff briefed each participant and recorded a written consent to use the assessment and intervention data. The participants’ personal information was de-identified, anonymized, and only designated researchers had access to the data.
1 Introduction
The spread of novel coronavirus 2 (SARS-CoV-2), also known as COVID-19, has changed the world and led to unprecedented global lockdowns and state of emergencies. India has the second-highest worldwide cases of COVID-19, with more than 11,409,831 infected and 158,856 casualties, a case-fatality rate of 1.5%, and a mortality rate of 11.2 deaths/100,000 inhabitants. (WHO, 2021). To counter the COVID-19 pandemic, the Indian Government pronounced a nationwide lockdown on 22 March 2020 for 21 days, which extended to 31 May with minimal relaxations. (Lancet, 2020). Even post-lockdown, the movement of 1.3 billion in India is restricted, enforced under the new normal, which encompasses social-distancing norms, strict hygiene practices, quarantine of affected people, and contact tracing exercises.
The shift to online teaching and work from home has helped tackle the virus’s spread during the pandemic. However, these measures have led to social isolation (Singh et al., 2020), increased stress (Rehman et al., 2021), anxiety (Rehman et al., 2021), depression (Rehman et al., 2021), and uncertainty (Serafini et al., 2020) in families, impacting children’s psychological and emotional development (Duan et al., 2020).
The most affected population group due to the preventive measures imposed to restrict COVID-19 spread are families who have children diagnosed with mental or physical disabilities (Marin et al., 2021), especially with Autism Spectrum Disorder (ASD) (Patel, 2020). Children with ASD struggle to adjust to routine change (NIH, 2021), have limited communication and social skills (Christensen & Zubler, 2020), and display restricted and repetitive behavior (Lidstone et al., 2014) that they find challenging to self-regulate (Amaral & de Vries, 2020; Eshraghi et al., 2020).
The sudden closure of schools, therapy, and daycare centers has prolonged home confinement and non-participation within communities for children with ASD, leading to increased aggression (Walsh et al., 2020), disrupted sleep patterns (Mutluer et al., 2020), increased restricted repetitive behavior (Williams et al., 2021). These unprecedented situations risk children and families acquiring additional mental health issues (Spain et al., 2021) and disrupting their emotional wellbeing (Alhuzimi, 2021; Courtenay & Perera, 2020).
Numerous studies suggest that parents of children with ASD display higher stress levels and low quality of life than parents of neuro-typical children (Hsiao et al., 2017; McStay et al., 2014). Amid COVID-19, family members of the children with ASD have taken household and professional responsibilities and played additional caregiver and therapist roles (Cahapay, 2020). The burden of additional responsibilities (Spain et al., 2021), lack of socialization amongst the community (Marin et al., 2021), and residential place usage amid work from home guidelines (Walsh et al., 2020) have added additional stress for families with no access to other supporting emotional or assistive resources (Spinelli et al., 2020). Parents’ stress can negatively affect their quality of life and lead to a stressful home environment impacting a child’s emotional and mental wellbeing.
In India, 1% of children less than ten years are diagnosed with ASD (INCLEN, 2018). Also, one hundred and eighty thousand new cases of ASD are added every year (Gokulakrishnan, V, 2021). The public healthcare facilities to handle ASD in India are limited, run overcapacity, and are located mainly in major cities (Sangath, 2017). During the pandemic, many services considered essential for families with ASD remained inaccessible (Mutluer et al., 2020; Singh et al., 2020) as most public-health facilities are reassigned to serve COVID-19 patients (Forbes, 2020).
The majority of schools and intervention centers in India have moved to Telehealth to serve children with ASD (Manral, 2020). However, there are several limitations to execute Telehealth-based ASD interventions in developing economies such as India. These include limited internet connectivity (Sengupta et al., 2020), technical bottlenecks, lack of professional therapist training to deliver the online intervention (Sivaraman et al., 2018), incompatibility of Telehealth platforms with assistive technologies (Patel, 2020), and lack of data security standards (Solomon & Soares, 2020). However, online interventions during the pandemic for preschoolers with ASD have led to improvements in general adaptive functioning (Martina et al., 2020) and promoted the adoption of Telehealth as a cost-effective long-term solution (Camden & Silva, 2020).
Studies have pointed to parents taking a prominent role in delivering home-based interventions for children with ASD using assistive technologies during the pandemic with observable outcomes (McDevitt, 2021). Narzisi (2020) has recommended ten easy steps that parents of children with ASD can practice at home, including structure, routines for daily activities, online-therapy, gaming, and semi-structured play sessions. Cahapay (2020) reported five Filipino parent experiences who successfully managed to home school their children with ASD amid the COVID-19 situation. Majoko & Dudu (2020) have highlighted parental roles in managing maladaptive behaviors and shaping new pandemic-associated essential hygiene behaviors such as hand-washing and wearing masks.
Interventions facilitated through mobile applications with parents’ assistance can complement Telehealth-based interventions. Mobile applications such as MITA, BUITIS (Aziz et al., 2019), and TOBY (Venkatesh et al., 2013) during pre-pandemic periods have enhanced parents’ skills to manage home-based interventions, improving language and vocabulary skills in children with ASD. However, intervention delivery has a high dependency on clinicians for program recommendation, personalization, and development of associated training resources and tools.
New generation machine learning technologies have shown promises amid the pandemic in the management of COVID-19 condition in patients (Alimadadi et al., 2020) by augmenting the clinician capacity (van der Schaar et al., 2020) and monitoring the mental wellbeing of students (Khattar et al., 2020).
The current study has two parts. Part 1 is a pilot study to measure the efficacy of an ABA intervention facilitated through a mobile APP via a change of SRS2 (Social Responsiveness Scale 2 ) scores for fourteen participants over 16 weeks intervention period. The part 2 study evaluates ABA intervention personalization capabilities of Artificial Intelligence algorithm on retrospective intervention data over one year for forty-four participants.
In the paper, we answer three research questions.
RQ1. Can a parent-mediated ABA program on a mobile application reduce Autism severity scores in children with Autism?
RQ2. Can Machine learning technologies personalize the child’s plan based on the pool of children’s longitudinal data?
RQ3. Can the machine learning technologies perform consistently on multicultural and multi-country datasets?
2 Applied Behavior Analysis Intervention
Sandback et al. (2021) reported seven early intervention methods concluding behavioral interventions as the promising method for children with ASD. Timely access to behavioral interventions is essential, as interventions administered to children between 12-48 months can maximize skill gains due to the brain’s high neuroplasticity (Towle et al., 2020). Applied Behavior Analysis (ABA), a gold standard intervention, has shown improvement in intellectual quotient (IQ) (Dixon et al., 2019), Socio-emotional and communication (Tiura et al., 2017), social-skills (Yu et al., 2020), and reduction in problem behavior (Rafiee & Khanjani, 2020) for children with ASD. Intensive ABA intervention lasting for more than two years in children has shown positive outcomes in the treatment group compared to the control group (Lotfizadeh et al., 2020).
India’s infrastructure for early intervention services is fragmented, overburdened with patient load (Sangath, 2017), lacks skilled clinicians, and has no insurance coverage (Helkkula et al., 2020) and therefore results in high treatment cost for the families (S Prakash, 2018). With fewer than a hundred certified ABA specialists (Board Certified Behavior Analyst Registry, 2021) in India, the quality, access, and affordability of evidence-based early intervention methods have limitations. The limited infrastructure and clinician availability lead to a twenty-month delay (Preeti et al., 2017) for families to access intervention services post first meeting with a professional. The pandemic has further limited access to early intervention services reducing the intervention benefits (Dawson, 2008) for children warranting an urgent contactless intervention services model for families diagnosed with ASD.
Traditionally, clinician facilitated, parent-mediated mobile-based ABA interventions (Novack et al., 2019; Parsons et al., 2017; Zaine et al., 2019) have promoted skill acquisition and have reduced ASD severity in children (Heitzman-Powell et al., 2014). Amid COVID-19, an amalgamation of parent-mediated, technology-driven ABA-based interventions can augment family members to play a caregiver role in ASD management.
3 Machine Learning
Machine learning technologies (ML) without being explicitly programmed can automatically identify patterns in multi-modal datasets and make decision outcomes for complex healthcare problems. Supervised learning methods using the classification approach learn from labeled datasets and can perform diagnoses and treatment recommendations for complex health issues such as stress (Subhani et al., 2017), and post-traumatic stress disorder (Wshah et al., 2019), depression, schizophrenia, and Alzheimer’s (Shatte et al., 2019). Unsupervised learning techniques such as clustering uses unlabeled data samples to detect Medicare fraud (Bauder et al., 2018), perform disease and patient subgrouping (Wang et al., 2020) from electronic health records, enhancing the efficiency and capacity of health care infrastructure.
Machine learning technologies are applied widely to make an early diagnosis of ASD. Wall et al. (2020) reported training of a machine learning algorithm, ADTree, to detect Autism in individuals with >99% accuracy in less than 72.4% of the time required using traditional methodologies. Deep Neural Networks (DNN) can learn patterns from unstructured data such as videos, images, and texts. DNN is implemented to measure behavioral landmarks from video sequences of participants to classify individuals with ASD (Vabalas et al., 2020), detect stereotypical behavior patterns (Silva et al., 2020; Zunino et al., 2018), and measure functional skills (Pandey et al., 2020). The ML technology has successfully resulted in shortlisting a minimal set of behavioral markers useful to make ASD diagnoses (Kosmicki et al., 2015), distinguish ADHD and ASD (Duda et al., 2016), and use home-based questionnaires and videos for early detection of ASD (Abbas et al., 2018).
Linstead et al. (2017) applied linear regression on a dataset of 1468 children. They concluded that an ABA intervention’s intensity and duration positively contribute to a child’s acquiring new skills, especially in academic and language domains.
Methodology
Methodology
2.1 Part I (Pre-Post design)
In the first part of the study, we used pre and post-intervention study design to measure the efficacy of parent-mediated ABA intervention facilitated through a mobile application.
2.1.1 Study Participants
Fourteen participants diagnosed with ASD aged between 2.5-8 years (mean – four years, ten months) were recruited in March and April 2020 through advertisements posted on social media. Participants were enrolled if they fall between the age-group of 2-8 years, have a diagnosis of ASD, access to a smartphone, and should not be taking behavioral interventions through another provider. We recorded informed consent, in-depth case history, and baseline SRS2 assessment scores for each participant during the enrollment phase.
2.1.2 Case Managers
Four case managers with a master’s degree in psychology and one year of ABA therapy experience under a Board-Certified Behavior Analyst (BCBA) were allocated to the parents. Each week, the case managers attended a 1.5-hour group meeting with a BCBA to discuss children’s and families’ progress and challenges.
2.1. Intervention Process
The participants enrolled in the study for sixteen weeks post-study brief and consent recording. The first meeting between case-managers and parents lasted for two-three hours. The case managers interacted online with families and recorded case-histories, semi-structured interviews, and baseline assessments on the Social Responsiveness Scale (SRS2). The case-manager developed a personalized ABA program that included six-eight skill-enhancement targets in communication, academic, and behavior management domains. The program targeted improvements in eye contact, imitation, gross and fine motor skills, object matching, independent play, completing puzzles, sorting shapes, and communication using pictures, gestures, and voice.
For each skill-enhancement target, a detailed lesson plan, training videos were added on the mobile application and personally explained. The plan was available to families on mobile applications with clear TO-DO instructions to follow in the morning, afternoon, and evening timelines and with provisions to record the child’s performance data. During weekly consultation sessions, the case-managers trained parents on reinforcement, prompting, prompt-fading, Discrete Trial Training (DTT), and task analysis. The training also covered how to access mobile application programs, record intervention responses, behavior instances, and communicate with the case manager. During weekly follow-up consult sessions, the case-manager took the therapy session’s feedback and reviewed the video and session-specific data available on the mobile application to revise, modify or create new therapy targets. The targets, once mastered, were revised by the case-managers to advanced skills from the 21 domains such as receptive and expressive language, object labeling and pictures, academics, classroom skills, and advanced comprehension.
For the intervention to be effective, the ABA program needs regular revision and personalization (Hyman et al., 2020), largely dependent on the case manager’s experience, knowledge, and complex decision-making (Ackley et al., 2019), and subjective process. These limitations warrant the use-case of adopting ABA program personalization using machine learning technologies.
4 Study Design
Pre-Post scores of the SRS2 scale were recorded for all fourteen study participants.
Fig 1. Study design for the first phase of study
2.2.5 Measurements
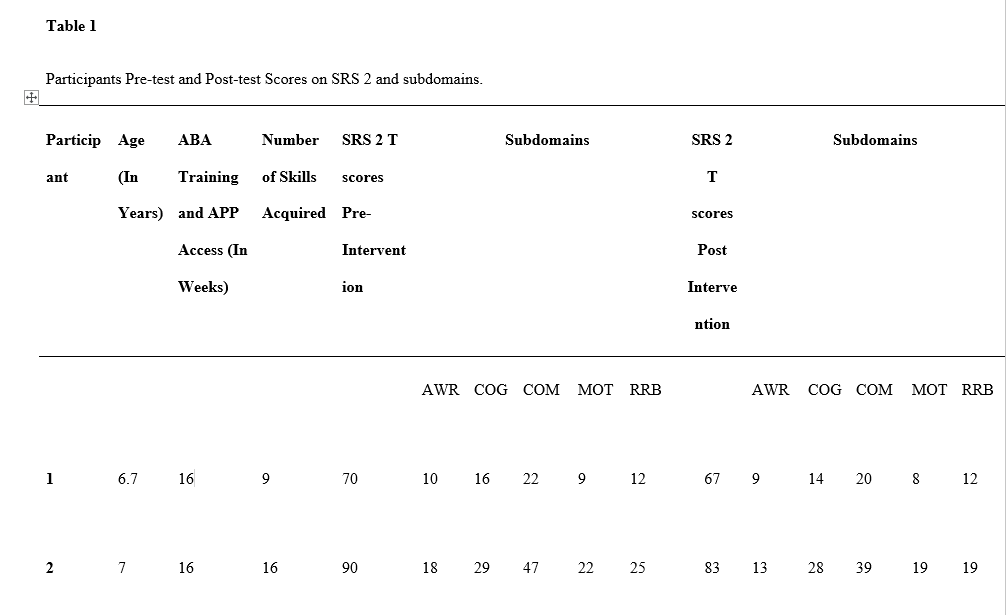
Table 1
2 Part II (Longitudinal Study)
We collected retrospective longitudinal ABA intervention data and applied machine learning models to personalize intervention plans. It is common to use retrospective data to train machine learning models and validate them on unseen data using the cross-validation technique.
2.2.1 Participants
We collected retrospective intervention longitudinal data for 44 children aged between 2-8 years from 2018-2020 who underwent an ABA intervention for a minimum of four months from Indian and USA ABA clinics. The available data included 24 children from the USA with an average intervention duration of 221 days and 20 from India with an average intervention duration of 195 days.
We trained machine learning models to one thousand one hundred and eleven intervention line items to develop an ABA program recommendation model. We validated the outcome using the cross-validation technique.
2.2.2 Behavior Technicians
Registered behavior technicians in the US and clinical psychologists with master’s degrees in India worked under Board Certified Behavior Analyst (BCBA) in center-based settings. They used ABA procedures such as operant conditioning, reinforcement, shaping, chaining, and prompt fading techniques.
Fig 2. Study design using the longitudinal therapy data for Phase II of the study.
2.2.5 Measurements
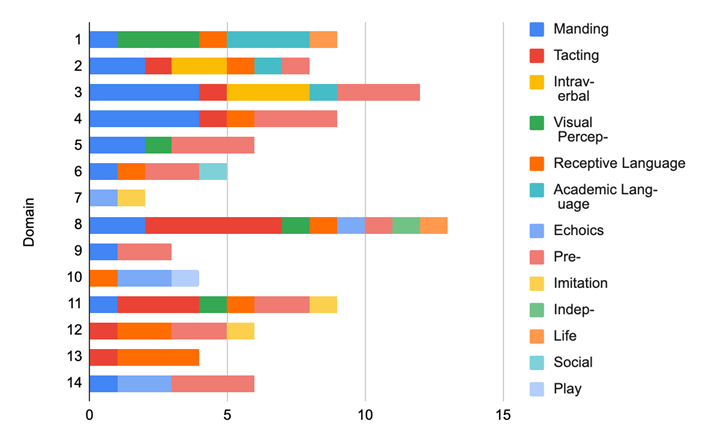
The mobile application used in the study ‘Cogniable’ allows intervention program recommendation and data-recording at the domain, target-area, and target level.
The application has 21 domains, such as tacting, manding, expressive language, imitation, and receptive language. Target-area is part of domains arranged in chronological order of easy to the difficulty level. For example, the imitation domain may consist of target areas as gross motor, fine-motor, imitation with objects, vocal imitation, and spontaneous and generalized imitation. The target is a sub-part of the target-area arranged in easy to difficult order level and is a skill taught to the child. For example, the target area fine-motor consists of imitating fine motor action, imitating drawing basic shapes, and imitating fine-motor action with the object.
We trained Machine learning models on the longitudinal data arranged as a feature set in table 3 to develop a recommendation model at the target area and target level. The feature set included the child’s age, targets mastered by the child in chronological sequence, and days to mastery. We included two additional skills in the feature set for each mastered target , selecting the previous two targets on a combination of a domain and a target area. We calculated days to master for targets in an intervention stage as an average number of days for a domain. However, techniques such as linear-regression can better estimate days to mastery.
We trained four machine learning models on the interventional data. Random Forest, Ada Boost, Gradient Boosting, and Naive Bayes,
Random Forests (Breiman, 2001) are a combination of tree predictors. Each tree depends on a random vector’s values sampled independently and with the same distribution for all trees in the forest. The prediction accuracy increases using the mean of the decisions of every tree, reducing model overfitting.
Boosting is a technique employed in weak prediction models. A sequential prediction for each stage is recorded, learning from the previous predictors’ mistakes, thereby improving the outcome.
In Gradient Boosting (Friedman, 2001), we repetitively leverage each iteration’s best outcome to create a more robust prediction, reaching the gradient convergence much quicker.
Naïve Bayes (Webb, 2010) finds out the probability of an event happening, given its related event already happened, assuming that one feature’s value is independent of the value of other features.
Finally, Ada Boost (Freund and Schapire, 1999) is mainly used to significantly better the accuracy of any low-performing algorithm. It refers to producing a very accurate prediction rule by improving the classifiers and their respective mathematical parameters by combining rough and somewhat inaccurate thumb-rules.
3.1. Phase I
In the first part of the study, the ASD severity scores measured on SRS2 scaled dropped post-intervention. Results of the pre-test SRS 2 (M = 75.8, SD = 10.44) and post-test SRS-2 (M = 71.77, SD = 10.27) suggest that the treatment resulted in a reduction of Autism severity on the SRS-2 in the sample.
The t-test scores were 4.67, p-value = 0.00054 , Cohen d =.39, t (49) = 115.44, p <0.01.
The statistical validation was done using python. The python line code to calculate t-test on the two related samples, ‘PRE’ and ‘POST’ (indicating the Pre and Post SRS-2 scores)
The p-value of the test is smaller than 0.001, which is less than the significance level alpha (usually considered 0.05).
Typically, we interpret Cohen’s D in terms of the relative strength of the treatment. It was suggested that d=0.2 is a ‘small’ effect size, 0.5 is a ‘medium’ effect size, and that 0.8 is a ‘large’ effect size. (Cohen, 1988). Thus, if the mean scores of the two groups do not differ by SD 0.2 or greater, the difference can be considered insignificant even if it is proven significant statistically. To further validate the findings, Cohen’s D was calculated.
Non-parametric statistical methods do not assume a specific distribution (such as Continuous, Pareto, Gaussian, etc.), hence we used one to verify whether, and how much, they did belong to different score distributions. The Wilcoxon signed ranks test (Wilcoxon, 1945) is a non-parametric statistical procedure for comparing two paired or related samples. The parametric equivalent to the Wilcoxon Signed Ranks Test goes by names such as the Student’s t-test, t-test for matched pairs, t-test for paired samples, or t-test for dependent samples.
Our study findings were rated at Statistics=0.000, p=0.001. Considering the usual value of alpha = 0.05, the p-value is below the significance level, and the samples are drawn from populations with differing distributions.
3.2. Phase II
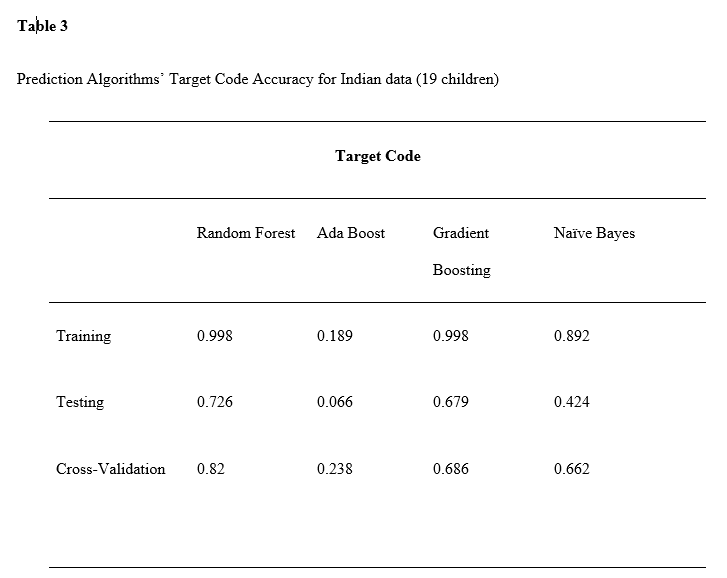
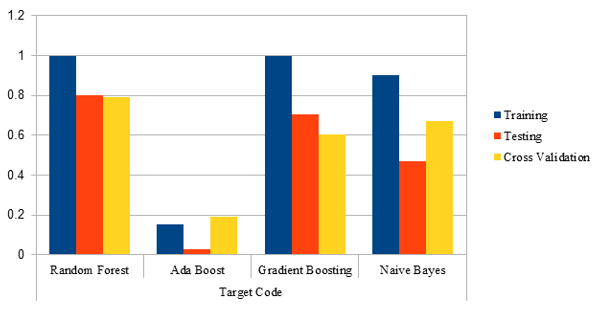
The post-training accuracy of each of the four trained algorithms are as follows:
Table 3
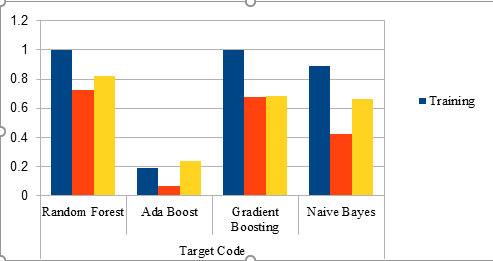
Prediction Algorithms’ Target Code Accuracy for Indian data (19 children)
Fig 4. Bar graphs representing accuracy results of Target Code Training, Testing and, Cross-validation phases for India data
Table 5
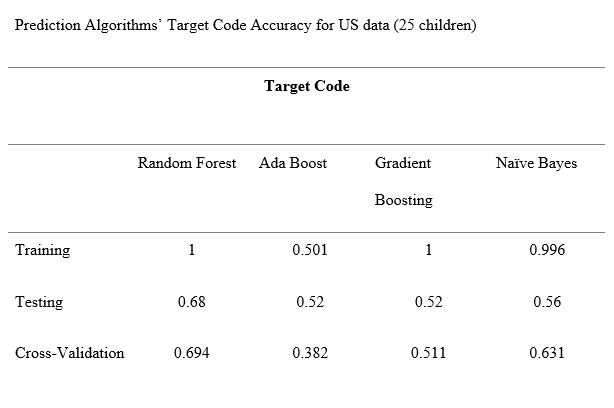
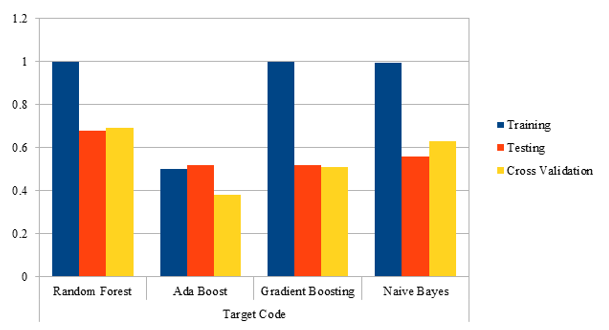
Prediction Algorithms’ Target Code Accuracy for US data (25 children)
Fig 6. Bar graphs representing accuracy results of Target Code Training, Testing and, Cross-validation phases for US data
Table 7
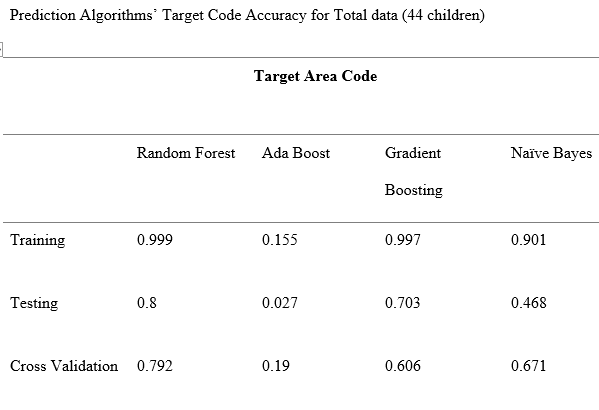
Prediction Algorithms’ Target Code Accuracy for Total data (44 children)
Fig 8. Bar graphs representing accuracy results of Target Code Training, Testing, and Cross-validation phases for Total (US+India) data
The Random Forest model has consistently predicted target recommendation for Indian, US, and combined population with a cross-validation accuracy of XX, YY and ZZ%.
4.0 Discussion
Post diagnosis, the use of ABA appears to be a feasible alternative for families awaiting EIBI services. Furthermore, the remaining literature on family outcomes during the post-diagnostic period reaffirms the need for such initiatives. The interventions focus on increasing the frequency, form and function of communicative acts.
The part-1 of the study was executed amid a pandemic in an in-home setting where the parents, mainly mothers, were the primary interventionists trained by the case-managers. The program had reasonable retention rates as fourteen out of sixteen families completed a sixteen-week intervention, and two families dropped due to stress and personal issues.
Three families during the recruitment phase responded to social-media advertisements and expressed interest in attending the study but had already begun receiving online behavioral interventions with private clinics in telehealth mode and therefore could not participate. The number of children with ASD enrolled in the current study (part 1 or part 2) outperformed the existing literature numbers, considering the situation amid COVID-19 and novel technology usage (Lazar, Feng & Hochheiser, 2017). Pre and post-intervention SRS2 scores were used to measure two paired T test for the participants.
The case-managers developed personal relationships with the families and recorded informal feedback that suggested ABA intervention training suitable and effective for families. However, most parents reported the intervention’s benefit and expressed concerns about the ease of integrating it into their day-to-day living during the pandemic. However, most recommendations for improvement focused on the frequency, schedule, and adaptations of the intervention protocol using play-based methods. Small, ad-hoc adaptations of program content were needed to meet the individual requirements. However, the case-manager and families’ feedback indicated that both the parties could handle these circumstances without requiring major revision in the intervention protocol. Overall, coaches and parents alike stated that they would recommend this intervention to others. Approximately 60 % of families undergoing the scheduled intervention program completed the daily task schedules.
The researchers came across many advantages of CogniABle Mobile application.
First, the case-managers could perform remote evidence-based assessments and build a personalized ABA program using the click of the button searching through domains, target-area, and targets arranged in chronological difficulty level. For each target in the child’s program, readymade resources such as lesson plans and videos required the case manager’s minimum time to adapt the program as per the child’s need. As per the family members’ availability, targets were incorporated in the morning, afternoon, and evening schedule and allocated to different family members such as siblings, parents, and grand-parents for execution. The common feedback received from the families was to make the mobile application, lesson plan, and video resources available in Hindi and other regional languages.
The use of the app ‘CogniAble’ during ABA therapy sessions helps make the intervention easier for families. The families could use resources and allow caregivers to perform more intensive interventions at their own convenience. Since ABA interventions heavily rely on regularly updated research and plausible data, researchers in this study collected real-time data on the participants’ learning skills and learning trends. Traditional data-analysis methods are time-consuming. However, CogniAble allowed clinicians to access the data efficiently, analyze child’s progress and make informed decision making on goal revision.
The participants showed improved communication skills as the interventions progressed. Even the three children who left the program at the end of 12 weeks due to personal reasons demonstrated improved skills in expressive and receptive communication. A meta-analysis of scientific literature provides evidence on ABA intervention on adaptive behavior, communication, interaction, comprehensive language, daily living skills, expressive language, overall intellectual functioning, and socialization. (Ospina et al., 2008). As every child with Autism is unique because improvements in abilities are subjective, especially in children with low-functioning Autism. The vast data collected through this intervention study can identify new indicators with statistical significance, especially by integrating advanced machine learning models to recommend and personalize intervention plans. The majority of families in the program reported rising problem behavior in children amid pandemics. The case-managers trained families to record duration, frequency, and ABC data in-home settings and guided them on basic steps to manage problem behavior.
. There is early evidence demonstrating the influence of advanced care training for mothers in helping children with ASD. In the same era, clinic-based services were also changed into family-based services (McConachie et al., 2000). Interventions which were perceived as acceptable to procedures and goals were more likely to elicit continued participation from the respective families (Carter, 2010; Wolf, 1978). Similarly, service providers, i.e., the therapists who perceived these interventions as admissible, are more likely to implement these with fidelity, which in turn can be linked to efficacy (Carter, 2010). Since there is limited literature on providing remote services to increase mothers’ capacity with ASD, we are hopeful that this study should act as a building block for future researchers in the same arena.
The retrospective data for part-2 of the study was collected from clinics where trained therapists performed the intervention. The collected data was transformed into the data-model of the mobile app Cogniable. Machine-learning models were applied to develop a therapy recommendation model for clinicians to personalize and revise the intervention plan.
Machine learning methods are novel computational methods that include mathematical learning, statistical estimation, and information theories, automatically discovering useful patterns in large amounts of data. This method has the advantage of accurate and reliable prediction using data with vast numbers of variables and causal inference within non-experimental data sets.
The application of machine learning models on large datasets can reveal significant features such as parental age, birth weight, and sociodemographic variables in prognosis and planning treatment of children with ASD using longitudinal data. (Mirac et al., 2019)
4.1.1 Pre-post Online Human Intervention Study on 14 participants
Pre-Post scores of SRS2 and the mean scores of post-tests in the intervention group were measured and compared using a T-score analysis. The result show significant differences in the mean of post-test scores in the group
The present study is officially the first study amid a pandemic based on families since mostly they were the ones providing interventions. As previously mentioned, significant effects were reported in some studies. This might be due to the use of video conferences alongside web-based intervention. Therefore, adding video conferences may increase the effectiveness of these types of interventions on mothers’ mental health. This study also demonstrated that the mean scores of SRS2 of post-tests in the group were lesser than pretest scores. There was promising evidence in terms of ASD reduction by web-based interventions. However, the studies are required to be well-defined, more well-designed studies are needed to strengthen the evidence concerning the impact of web-based interventions on
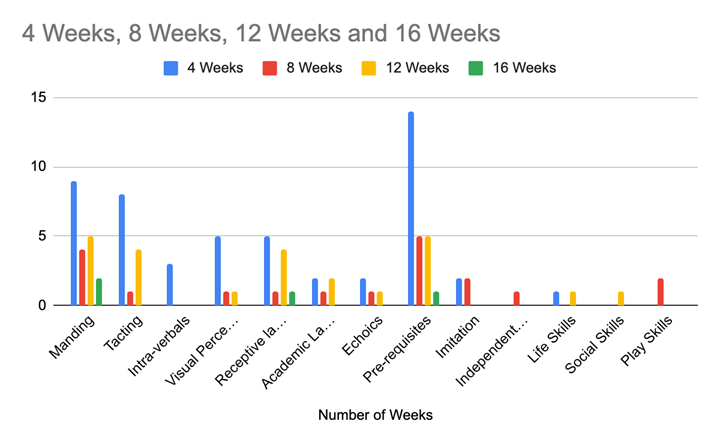
ABA skills. The study results also pointed out the children’s significant skills in ASD in multiple domains and how the participants mastered certain skills. Table 9 reports these skills and the number of participants who mastered them.
Table 8
Skills Mastered and Duration
Fig 9. Bar Graph representing Skills Mastered and Duration
Fig 10. Bar graphs representing skill acquisition of participants
4.1.2 Existing Longitudinal Study of Therapy on 44 participants
The part-1 of the study established the improvement in language and communication skills of children with ASD engagingly. This result coupled with previous literature suggests that ABA intervention plays a crucial role in skill acquisition and reduction in ASD severity. However, the scalability of the technology-assisted interventions can significantly enhance with the integration of machine learning technologies. In part-2 of the study, we used retrospective data for 44 children to personalize and recommend ABA intervention to clinicians enhancing their capacity.
5.0 Limitations
Even though pre-post study design is beneficial in comparing an intervention’s effectiveness, it has some drawbacks. The interpretation of pre-post intervention studies is difficult due to the lack of a control group.
Changes in the outcome of interest, for example, reduction in ASD severity, maybe due to the intervention; however, it may also reflect other reasons such as disease natural improvement, the motivation of parents to deliver the home-based intervention, availability of family support, educational background of families engaged in delivering the intervention and patient selection (patients before and after the intervention may have differed in clinically important attributes). Also, there is a natural tendency for processes to regress to the mean, which may occur without intervention.
Additionally, this study has some more limitations that must be taken into account. First, the small sample size and the non-homogeneity of the sample were due to the challenge of enrolling ASD children online amid pandemics, who shared similar functional and behavioral profiles. The small sample size was further reduced for some measures that were only administered to a subset of parents, for example children with advanced skills. The case-manager faced another setback when two of the participants dropped out of the intervention due to stress from the lockdown amid the Covid-19 pandemic. As with any research based on informed consent and voluntary participation, a degree of sample bias was not excluded. Second, the study outcomes concerning skill acquisition, SRS2 assessments were dependent on the respondents, making testing the app’s efficiency and efficacy challenges. However, the families were selectively recruited, who had already been without support amid the pandemic. Given their situation, their reaction to the intervention may not represent the experiences of families who will ultimately be eligible for ABA as a whole. Since each individual with Autism is unique and has specific abilities, progress and learning trends are very subjective and depend upon external factors such as family, health conditions, environment, and others. Being a relatively short study, our findings, although encouraging, cannot yet represent the population of preschoolers with Autism. Along with this, certain types of behavior may have been overexpressed or otherwise not expressed in our sample, thus making it difficult to generalize the outcomes. Third, some measurement bias could have been introduced. It is also important to consider what kind of treatment the child and/or family were undergoing in a public or private health structure. In our sample, the intervention was performed in the pilot test. Another aspect considered was whether the training conducted by case-managers had expertise in the correct use, demonstration and mobile app training. We did not measure the software training fidelity as part of this feasibility assessment. The flexibility of the CogniAble further carries the risk of sessions being improperly conducted, for instance, changing level or program at the wrong time for the needs of the child; thus, the present pilot study did not report on treatment fidelity. However, it is important to evaluate each child’s progress since this can provide indications for future research.
Another imperative yet possibly overlooked aspect of identifying ASD and improving the child’s cognitive capabilities is the quality of parenting and parents’ mental health during this challenging process. We had not measured the mental well being of families (Green et al., 2017; Oono et al., 2013), sense of competence amid pandemic (Abouzeid et al., 2019). Furthermore, our study took into account the Indian culture, within which most of the caregivers of children with ASD were mothers. So, the design might not be well-suited for fathers and other family members of children with ASD responsible for caring for these children. Also, in the present study, it was not possible to record the number of hours mothers spent on the Mobile APP, i.e., a lack of information on how much time was taken to download the information and its usage. During the second phase of the study, we utilized multicultural data, which may hinder model training. However, based on our results and a study was done by Zhou et al. (2019) the concerns regarding the negative impact of multilingual/multicultural data are alleviated. Hence, the algorithm could adapt to the multicultural data and provide personalization recommendations in a much better way. There is no in-person interaction with the therapist for them to see improvements in person while interacting with the client themselves could be seen as a potential drawback in some cases.
Irrespective of these limitations, this study attests to the feasibility and acceptability, at an organizational level, of the parent coaching intervention based on the ABA in a real-life community setting as an interim service offered amid pandemic.
6.0 Future Research
Based on what we learned from the successes and limitations, future replication studies with a larger sample size, longer duration, and more variables in the equation must be conducted to investigate our results’ significance. Wide-scale implementations of the program that can accommodate a greater number of participants and promote early access will substantiate our findings. Future implementations of the ABA therapy should also evaluate parents’ teaching skill performance early as the first session and continue to monitor it throughout. Comprehensive and detailed, regular feedback will ensure better results. Interventions that support parents in this manner should ultimately improve the quality of EIBI (Estes et al., 2014). An important step in this will also be to formally examine parents’ mental wellbeing and how that contributes to their skills. Furthermore, case-manager knowledge related to software could be included in future studies to identify barriers that hinder implementation in other socio-economic settings.
We selected the SRS2 because it is easy and fast to administer online and has been used to study the needs of individuals with ASD in various instances. (Prado, Magalhães, & Wilson, 2009) Further studies should be guided using standardized motor performance tests delivered by qualified professionals for corroboration and replication of our findings, potentially in other countries. In the present study, it was not possible to take into account caregivers’ experiences. Overall, the present study yielded promising results in terms of the implementation process. The recruitment of qualified staff through the other community-based organizations allowed for the optimization of available and competent human resources. Although the staff was from varied educational and disciplinary backgrounds, they were adept with ASD and ABA-based principles. This suggests that these types of programs can be integrated into primary care settings. They are consistent with the available resources in India’s public network of primary healthcare and social services. Also, the AI model’s personalization capabilities may support long-term engagement, as therapists could validate the program proposals to each child’s needs and capabilities on that particular day of the intervention. This would reduce human bias in even the most experienced clinicians and further fine-tune the model. A crucial factor in these interventions succeeding was the clinician’s close collaboration with the participating parents.
During the test period, the parent’s involvement was not sufficient for the protocol’s needs. For future references, for these kinds of studies to be even more successful, it is recommended that the parents receive specific training in advance. Reaching out after the diagnosis, extending the recruitment interval, offering sessions at different times of the day, and adding a babysitting service for siblings could be realistic adaptations to encourage more families to sign up for such studies in the future. It is also suggested that future studies pay attention to mothers’ experiences and work on incorporating fathers and other family members as caregivers. In some countries like India, the state education program is not equipped to support such interventions, and thus it would do good to make such programs more accessible and widely known. This would also help with the social acceptability of children with ASD and help them in their interpersonal relationships. The findings are thus promising. Along with other preliminary studies conducted by our team, we have set the stage for the third phase of evaluating the parent coaching intervention in an RCT.
As one of the ulterior motives of this pilot study was to evaluate whether children with ASD would benefit by using a technological approach , our findings have been useful for other researchers who are trying to conduct longer and larger technological interventions for children with ASD. These results should encourage research in clinical, assistive technology, and human-computer interaction for testing the long-term efficacy and efficiency of such technological interventions. Further research should also be conducted to improve the design of novel Mobile based technological interventions . These new designs could generate new knowledge to boost research in Computation and Neuropsychology.
To conclude, this research offers promising results regarding children’s actual learning abilities with Autism, suggesting that it would be worthwhile to investigate technology-enhanced learning in a fully controlled ‘safe’ (impeding self-stimulatory interaction with the technology) environment. This will help verify whether free interaction could further aid their progress over time.
7.0 Conclusion
The present study investigated whether ICT could enhance Applied Behavior Analysis rehabilitation therapy for children with Autism amid pandemics and integrate with a scalable machine learning model enhancing clinician capacity.
The studies also report that highly structured behavioral methods yield positive results for these children. Previous work in the field of ABA intervention reports that ABA programs and data analytics as separate components. The app used for this research, CogniAble, features both components integrated under one tool, receiving positive reviews from children and caregivers alike. The clinicians can save time through the app due to the rapid setup, personalization, and data monitoring functions. The saved time can thus be devoted to the learning intervention, allowing more time for mastery of more items in the same time slot.
Lastly, personalization, a crucial component for people with Autism, is implemented by integrating machine learning technologies.
s.
The above researched and designed mobile-based intervention can be used to provide daily care training for mothers of children with ASD. Thus, it can be concluded that CogniAble allows easy maintenance of the code and high accuracy of data collection since the tutor constantly evaluates the trials. Consistency and coherence of the intervention are fully assured; each tutor can automatically continue the intervention of the previous ones (3/4 tutors rotate) without needing to read the paper reports used in the traditional ABA sessions. As a result, the app improves the rapidity and accuracy of the intervention. Another advantage of the app was that the intervention provided was entirely over the internet, and there was no need for travel, pay, and continuing communication between the website’s supervisor and the mothers. Such interventions would prove to be time and cost-effective. Finally, it is safe to say that it can also be used by non-clinical personnel, thus sustaining families in their daily burden in rehabilitating children with Autism.